Upper limb spasticity is suffered by a full 70% of the stroke population, By three months post stroke 19% of people will experience spasticity and this figure increases to 38% of people after 12 months.
Did you know that it’s one of the biggest things that survivors tell consultants, GPs, family, carers and friends that they wish they could positively alter?
Spasticity can develops months or even a year after stroke — and often may become more noticeable as recovery moves on and can have a very significant bearing on your quality of life. Let’s look at what spasticity is:
 Muscle stiffness;
Muscle stiffness;- Upper extremity hypertonia (excessive muscle activity);
- Loss of fine motor control (for example small hand movements);
- Paresis;
- Soft tissue contracture;
- Muscle overactivity leading to the reduced ability to relax;
- Muscle spasms;
- Changes in limb posture; and
- Muscle fatigue.
Let’s see if you can grab some tips here to help you beat its limitations.
Spasticity is caused by miscommunication between your brain and your muscles. It has neural and non-neural components to it. Let’s delve deeper: knowledge is power,
Normally your muscles are in constant communication with your brain about how much tension they’re feeling, and the brain has to constantly monitor this tension to prevent tearing. Your brain continuously sends out messages telling your muscles when to contract and relax.
1st layer to spasticity:
When a stroke damages part of the brain responsible for muscle control, this communication is thrown off.
The damaged part of your brain no longer receives the messages that your muscles are trying to send, and as a result, your brain no longer tells them when to contract or relax.
So, your muscles keep themselves in a constant state of contraction in order to protect themselves.

2nd layer to spasticity:
While your muscles are always in communication with your brain, they’re also in communication with your spinal cord.
Usually the spinal cord takes the messages from your muscles and sends them up to the brain.
But since the brain is no longer reading those messages, your affected muscles have ‘nothing to talk to’.
So, the spinal cord takes over, but it doesn’t know how to properly operate your muscles. It really only has one goal: to prevent your muscles from tearing.
In order to do that, your spinal cord sends signals to keep your muscles in a constant state of contraction (flexion), which is what causes spasticity.
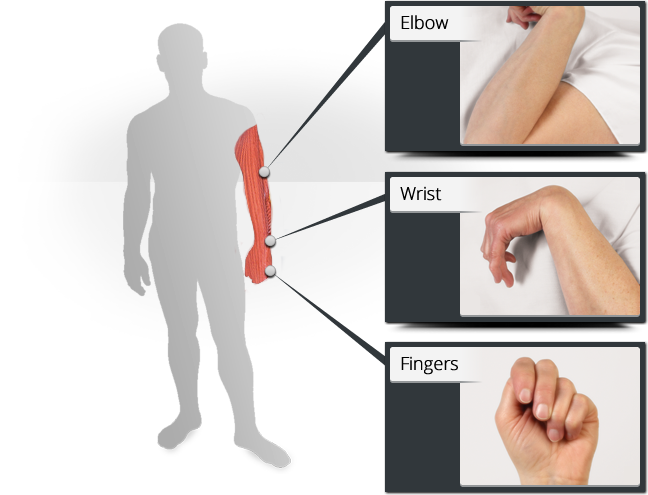
For instance, your spinal cord does not want your arm flapping about and becoming liable to be damaged, hence the typical pattern of spasticity of flexed elbow, wrist, finger and thumb joints that you may see others have or have yourself.
Your spinal cord has the best intentions; to prevent your muscles from tearing. But it’s frustrating because spasticity can cause muscles in your arms or legs to tighten uncontrollably, causing pain and discomfort. Certain muscles (such as the muscles that bend your fingers) can become continuously contracted. Spasticity depends on the speed with which muscles are moved. So, the faster a passive stretch is made, the faster your resistance to it will be.
Other symptoms may include clonus (a series of rapid muscle contractions), muscle spasms, scissoring (involuntary crossing of the legs), and fixed joints.
The degree of spasticity varies from mild muscle stiffness to severe, painful, and uncontrollable spasms.
Don’t think of spasticity as all bad though: although it may cause shortening, it is keeping your flexor muscles strong. This ‘spasticity strength’ can be used functionally too, in a number of ways, particularly to help you conduct tasks. It is very difficult to achieve reduction from spasticity. There is no global answer to eradicating spasticity.
However, a very good start at progressive spasticity decline work can be made via a mix of performing constant stretching in an effort to keep your muscles long, plus the introduction of an anti-spasticity drug if appropriate, plus a progressive task-training programme is a good start. I’ll show you a good way to do ‘task training’ below the very brief note about the injectable drug below.
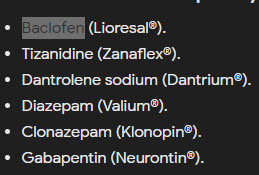 Examples of global (oral) medication are (trade names removed but see pic to the right), aim to relax your muscles by ‘turning down’ your nervous system. The downside of many of these is that they can also cause you to feel drowsy, confused, dizzy, weak, tired or to have a headache.
Examples of global (oral) medication are (trade names removed but see pic to the right), aim to relax your muscles by ‘turning down’ your nervous system. The downside of many of these is that they can also cause you to feel drowsy, confused, dizzy, weak, tired or to have a headache.
An example is the second medication in the list, which helps with spasticity by stopping your muscles from spasming and it also ease pain.
Because it lasts for a short time, it is best used only when you need it for relief or to be able to complete certain activities.
An example of a localised medication is (trade name removed but see pic below).
It has been designed so that it can be safely injected directly into target sites to block the nerves from sending messages to the muscles, causing them to relax. The evidence shows that it decreases spasticity, but likely does not improve upper limb motor function. But still, it is worthwhile having if your consultant considers that it is appropriate that you go for assessment.

If you go for this, ask if the injection(s) will be guided by ultrasonography rather than by electrical stimulation or palpation. Also, it is easy for the injection to limit existing useful underlying motor movement from occurring, so care needs to be taken and a robust physical training regime must be in place before injections in order to maximise efficacy.
Further, in combination with electrical stimulation or modified constraint induced movement therapy, it is possible that you are likely to improve muscle tone in your upper limb, although advice MUST be sought from your GP and/or consultant at all times.
So, what do you do to train your contralesional hand? First, think about the huge amount of repetitions you need to do. You have to. It’s the only way I personally got my upper limb back from a pattern of spasticity to virtual ‘normality’.
Training should be done every day: and a large daily amount of task-specific work is required. Repetitions.
So, you need a ‘go-to’ set-up in order to make this easy. Advised are my two best ‘go-to’s.
Advice: Stretching precedes tasks. and allows you to access them (particularly if you cannot sustain a gap between your thumb and forefinger. Successful stretching can also increase the number of repetitions available to you. So, STRETCHING ENABLES THE TASK. It also ‘EXTENDS TIME ON TASK.’ I detail all this in the Successful Stroke Survivor manual.
Kit-wise: an all in one ‘reverse gripper’ called Neurogripper which repetitively opens the hand in a gradated manner, combined with daily use of the Task Training Board, combined of course with testing progess via your activities of daily life, is a way to push your rehab to the next stage.
RECIPE TO DO DAILY TASK TRAINING – use hand stretch device Neurogripper with a Task Training Board





 The aim for this study is to research a treatment method to see if can improve upper limb function.
The aim for this study is to research a treatment method to see if can improve upper limb function.

 Stroke survivors simply tend to know when therapy seems to have ended too soon. They can feel very neglected. Let’s quickly examine Professor Glen Gillen’s handbook ‘
Stroke survivors simply tend to know when therapy seems to have ended too soon. They can feel very neglected. Let’s quickly examine Professor Glen Gillen’s handbook ‘





