Do you have shoulder dysfunction and/or pain as a result of your stroke, or know someone who does?
Studies estimate that 50% of stroke survivors experience proprioceptive impairments in their upper limbs. These may include limited range of motion, muscle weakness, joint instability, and pain, all of which can severely affect independence and quality of life and are interlinked with motor, sensory, and musculoskeletal changes.
Shoulder dysfunction and pain are among the most common and disabling consequences of stroke. Everyday tasks such as dressing, eating, or reaching for an object become difficult or even impossible. Balance and coordination problems are also prevalent and deeply interconnected with shoulder dysfunction. People recovering from stroke often experience fatigue, weakness, and joint stiffness that make conventional rehabilitation programs difficult to access or sustain.
 Shoulder pain
Shoulder pain
If you have hemiplegia in your arm from your stroke, there is a good chance that you may also suffer from shoulder pain. Shoulder pain can disrupt your daily activities and make it difficult to sleep. The shoulder is a ball-and-socket joint that allows motion in any direction. Because it’s so mobile, it’s also vulnerable to injury.
Some people have shoulder pain as early as two weeks after their stroke, but it’s more common for it to start about two to three months later. The evidence indicates that 80% of patients with post-stroke shoulder pain have resolution within 6 months. Shoulder pain can have consequences on not only the use of your arm and hand, but also other aspects of your rehabilitation, such as transferring from a bed to chair or maintaining balance.
There are many things that can cause shoulder pain including (but not limited to) poor arm function, spasticity, subluxation, bursitis, and tendonitis. Bursitis is a shoulder disorder that occurs when the bursa sac (the padding between the bones and tendons in the shoulder) becomes inflamed. In some cases, bursitis can lead to ‘frozen shoulder’; a condition that causes it to lock up, significantly affecting how much you can use it. You may be given a sling in hospital to try and reduce shoulder pain, but currently there is no clear evidence that sustained sling usage significantly corrects shoulder pain.
Shoulder subluxation
Shoulder subluxation is a partial (minor) dislocation of the arm at the shoulder joint that often occurs after a stroke. In most cases, extreme muscle weakness can result in the muscles not being able to hold the weight of the arm at the shoulder, resulting in the humerus (upper arm bone) dropping down out of the shoulder joint. It can also cause the shoulder blade to lose its normal position. Muscles affected by spasticity around the shoulder joint can also pull the humerus and shoulder blade into abnormal positions.

If your arm is affected by subluxation, your physiotherapists will let you know, and you may well be able to see the difference in level between your more-affected and less-affected shoulder in the mirror. It’s important to protect your shoulder from injury and try to keep your more-affected arm in as normal a position as you can manage.
When resting, your more-affected arm can be kept in a comfortable position which prevents or lessens subluxation. Make sure no-one lifts you from a seated or lying position underneath your arms. This can cause damage. Instead, try learning with a therapist, as soon as you can, how to get yourself from both a seated to standing position and from the floor to standing without involving your more-affected arm much.
There is evidence that starting with a sling suspension system and conducting active shoulder exercises may be effective in reducing shoulder subluxation, improving proprioception and upper extremity function. However, after discharge, survivors often retain slings for lengthy periods in the community simply because they have no clear guidance concerning whether it’s possible to reduce (or stop) using one altogether. And if so, when to do it. Please understand that a sling won’t help you in the long run and may well hold back your recovery.
Understandably, improvement of post-stroke shoulder subluxation is shown to improve performance of task-specific, functional activities. So, you must seek the advice of a therapist or your GP concerning how and when to reduce sling usage. Careful retraining without one is the probably the only way, combined with exercises such as those listed below, that you’re going to fully correct shoulder subluxation.
Range-of-motion exercises for the shoulder joint should include flexion-extension, abduction-adduction and external-internal rotation. Careful weight-bearing exercises for the affected upper extremity can be very beneficial for you but pulling motions, like rowing, must be avoided. Training with a linear shoulder robot can improve shoulder stability, motor power, and result in improved and retained functional outcomes. Electrical stimulation is also shown to be consistently effective at reducing subluxation…
 But what if therapy didn’t have to feel like therapy? An invitation extended to you if/as appropriate for you!
But what if therapy didn’t have to feel like therapy? An invitation extended to you if/as appropriate for you!
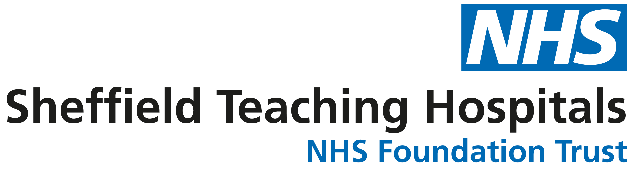
A New Way to Move: Non-immersive Virtual Reality Rehab from Home
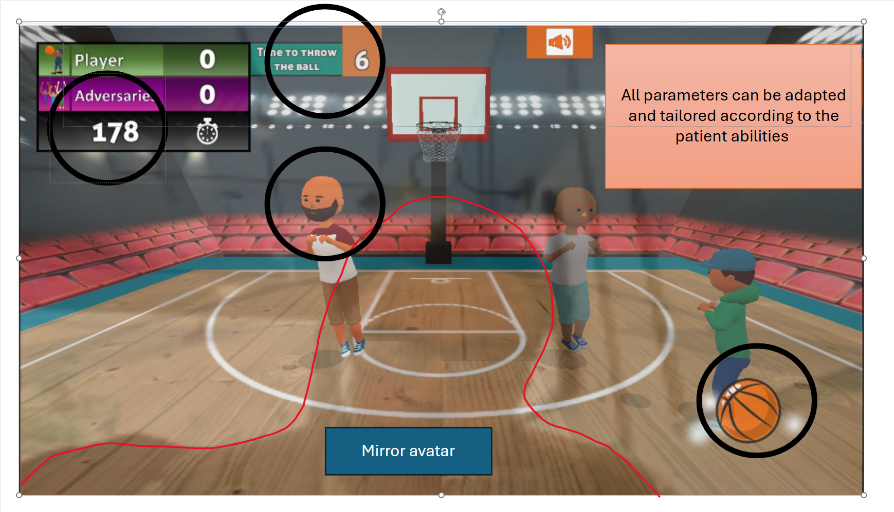
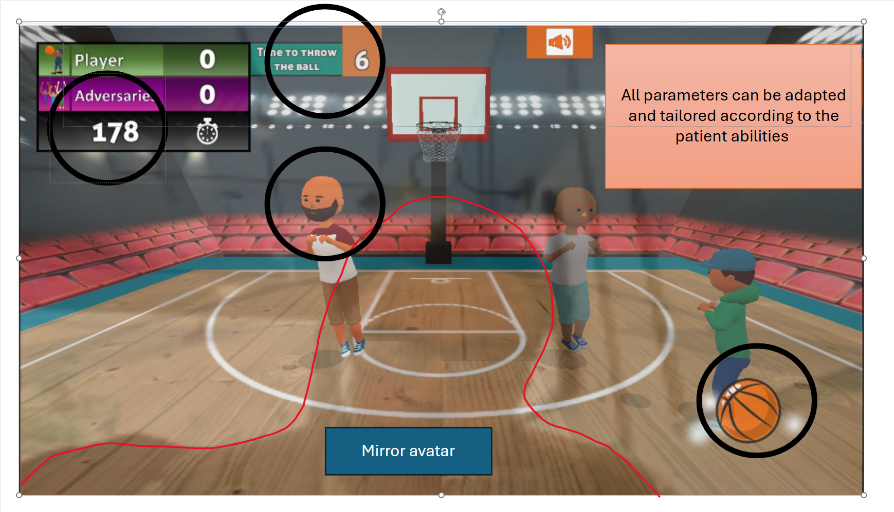
A collaborative team from University of Exeter and University of Leeds is exploring a novel solution: using a web-based game that can be accessed from any device with a camera to help improve shoulder movement, balance, fatigue, and pain in chronic stroke survivors.
The study is part of the eMBraCE activity programme, which aims to see whether digital, game-based exercises can help chronic stroke survivors regain shoulder movement and improve their balance while reducing pain and fatigue.
The idea is simple but powerful: deliver fun, engaging therapeutic activities through a game, allowing users to do short bursts of guided movement in the comfort of their home. No special equipment is needed — just a laptop, tablet, or smartphone with a webcam.
 This study is proof of concept that aims to see whether even short-term use of such a game can make a measurable difference. And now, they are inviting participants to get involved too.
This study is proof of concept that aims to see whether even short-term use of such a game can make a measurable difference. And now, they are inviting participants to get involved too.
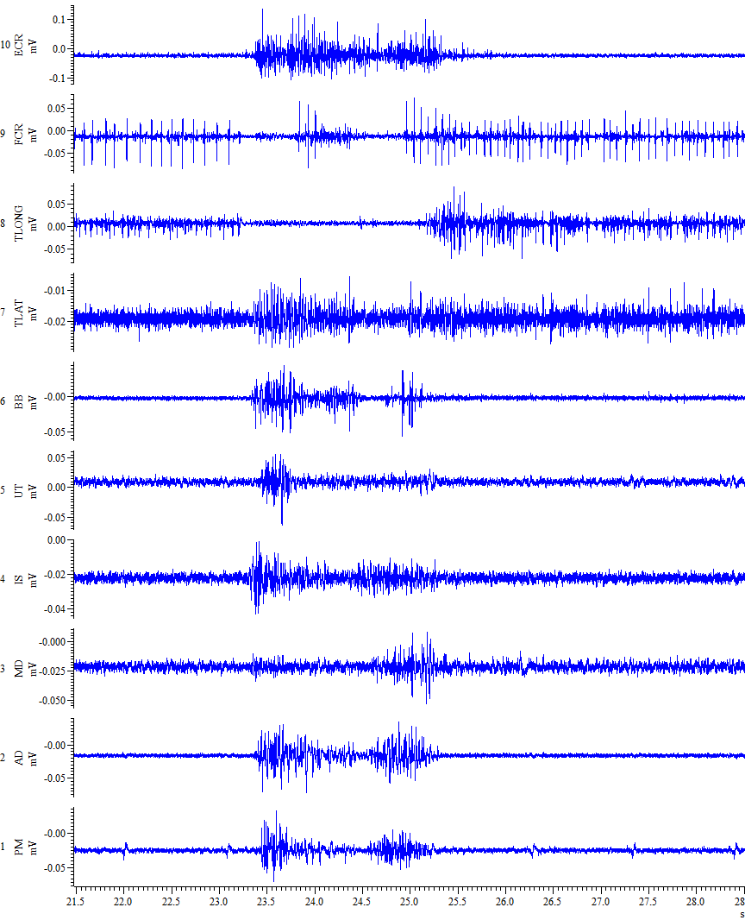
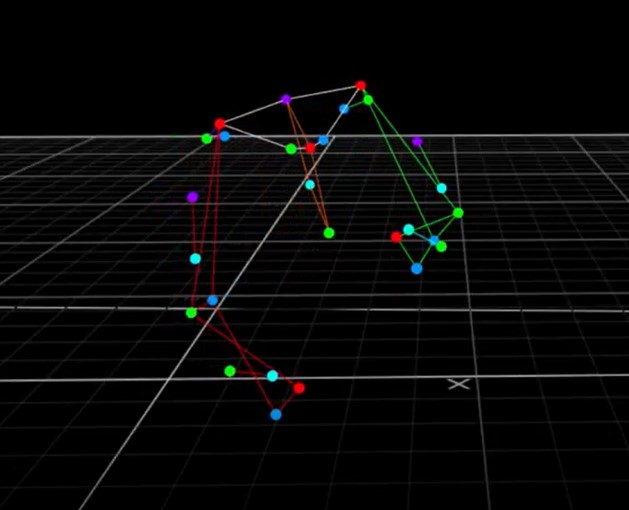
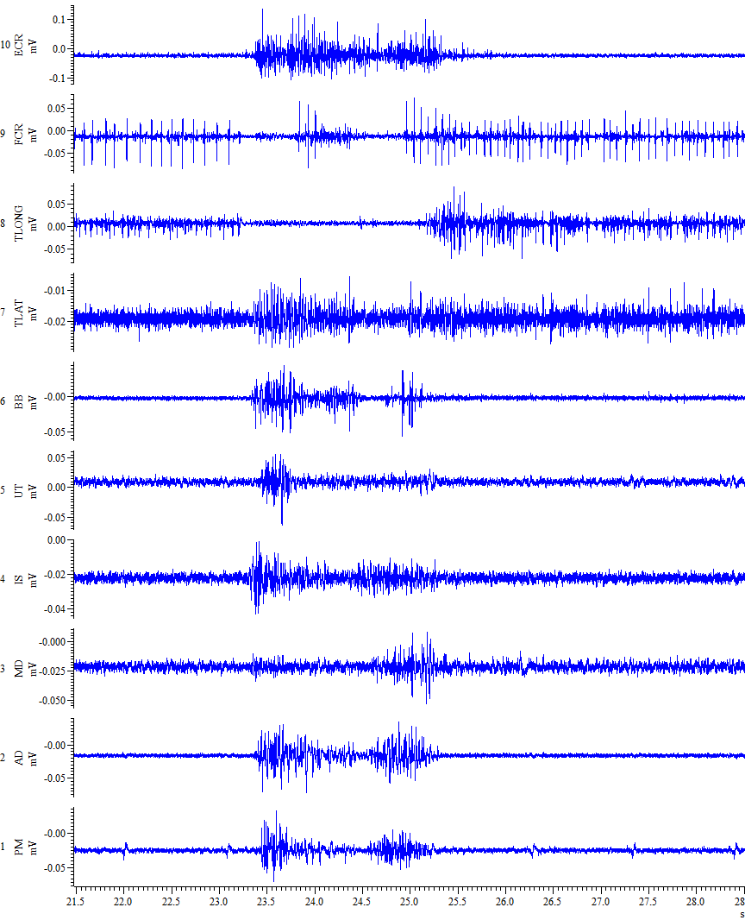
One of the things they will measure is electromyography (EMG) signals from the skin surface. This will tell them about electrical activity produced when muscles contract. They plan to use this to assess how the nervous system is adapting to control movement in different pain conditions.
Frequently Asked Questions (FAQ)
What is the purpose of this study?
This study is part of the eMBraCE activity programme. It aims to see whether digital, game-based exercises can help chronic stroke survivors regain shoulder movement and improve their balance while reducing pain and fatigue.
Who can take part?
You are eligible if:
- You’re aged 18 or over
- You are a stroke survivor, living with long-term effects
- You can walk independently, with or without a walking aid
What will I be asked to do?
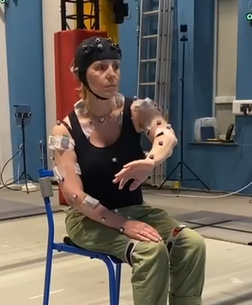 You’ll attend a session at the VSimulators facility in Exeter or University of Leeds. The session takes about 2 hours, including preparation and testing.
You’ll attend a session at the VSimulators facility in Exeter or University of Leeds. The session takes about 2 hours, including preparation and testing.
During the session they will ask you to:
-
-
-
-
- Wear some small boxes or wired sensors that measure your muscle activity
- Perform basic movements like standing, walking, turning, and lifting
- Use a web-based game designed to help guide shoulder and balance exercises
- Fill out questionnaires about your experience and symptoms
Are there any risks or discomforts?
Risks are minimal. You may feel some fatigue or mild discomfort during the exercises, similar to any physical therapy session. The team will be with you throughout to ensure your safety and comfort.
Will I be paid for taking part?
There is no payment, but the team offers up to £50 reimbursement for your time and travel costs.
How is my personal information handled?
Your data will be pseudonymised (de-identified) and stored securely. You can choose whether or not any images or videos taken during the session can be used in publications or presentations. Opting out will not affect your participation.
Can I withdraw from the study?
Yes. You may withdraw at any time, even during the session, and can request your data be deleted if you wish.
If you are interested in taking part or would like to have some more information feel free to contact study researcher Tom Richards: t.richards2@exeter.ac.uk
Dukelow, S. P., Herter, T. M., Moore, K. D., Demers, M. J., Glasgow, J. I., Bagg, S. D., Norman, K. E., & Scott, S. H. (2010). Quantitative Assessment of Limb Position Sense Following Stroke. Neurorehabilitation and Neural Repair, 24(2), 178–187. https://doi.org/10.1177/1545968309345267





 This study is proof of concept that aims to see whether even short-term use of such a game can make a measurable difference. And now, they are inviting participants to get involved too.
This study is proof of concept that aims to see whether even short-term use of such a game can make a measurable difference. And now, they are inviting participants to get involved too.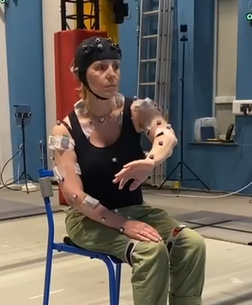 You’ll attend a session at the VSimulators facility in Exeter or University of Leeds. The session takes about 2 hours, including preparation and testing.
You’ll attend a session at the VSimulators facility in Exeter or University of Leeds. The session takes about 2 hours, including preparation and testing.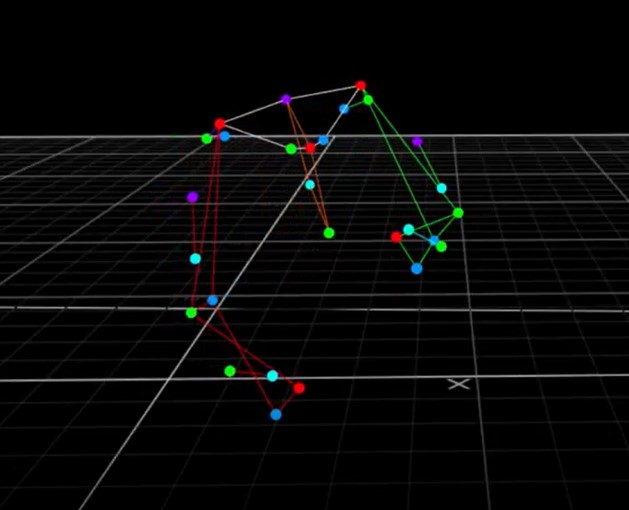
 Your GP no doubt has already told you that if he or she could put cardiovascular exercise into a drug, it would be one of the most effective medications to prevent and/or treat patients with cardiovascular and/or cerebrovascular diseases. But cardiovascular exercise, despite the known benefits, is still known to be under-utilised by clinicians as a ‘prescription’ during rehabilitation.
Your GP no doubt has already told you that if he or she could put cardiovascular exercise into a drug, it would be one of the most effective medications to prevent and/or treat patients with cardiovascular and/or cerebrovascular diseases. But cardiovascular exercise, despite the known benefits, is still known to be under-utilised by clinicians as a ‘prescription’ during rehabilitation.

 The evidence for exercise after stroke has resulted in the development of stroke-specific community exercise programmes. The system is analogous to the very well-established rehabilitation services for cardiac disease patients which usually start after usual rehabilitation has ended. Collaborations between health boards and council-run leisure centres have resulted in the establishment of exercise referral schemes, which have provided a range of stroke-specific cardiovascular exercise programmes delivered to smaller and larger groups.
The evidence for exercise after stroke has resulted in the development of stroke-specific community exercise programmes. The system is analogous to the very well-established rehabilitation services for cardiac disease patients which usually start after usual rehabilitation has ended. Collaborations between health boards and council-run leisure centres have resulted in the establishment of exercise referral schemes, which have provided a range of stroke-specific cardiovascular exercise programmes delivered to smaller and larger groups. Those that are known as recumbent or semi-recumbent bikes (depending how reclined it is) would be my first choice for a ‘beginner stroke survivor’. These types of gym bikes can be picked up relatively affordably from a variety of places and often aren’t cheap but they hold a considerable re-sale value.
Those that are known as recumbent or semi-recumbent bikes (depending how reclined it is) would be my first choice for a ‘beginner stroke survivor’. These types of gym bikes can be picked up relatively affordably from a variety of places and often aren’t cheap but they hold a considerable re-sale value.
 A big tip from Tom: make sure to record and celebrate any and all successes. Try to pinpoint how you achieved new action control in your ADLs. This is often via something achieved in your retraining. Start to become aware of these. Get this data recorded somehow.
A big tip from Tom: make sure to record and celebrate any and all successes. Try to pinpoint how you achieved new action control in your ADLs. This is often via something achieved in your retraining. Start to become aware of these. Get this data recorded somehow.
 Also, note as an aside that if ‘Press’ may involve ‘where one creates’ / where/who is around to help you do stuff / what sources can you look at / involve with etc etc, it does rather shine a light on the importance of being cognisant of not just ‘where one is’ (eg, in a flat, in a tower block, in the suburbs of London) but how one can bring maximal resources to bear to help your own situation.
Also, note as an aside that if ‘Press’ may involve ‘where one creates’ / where/who is around to help you do stuff / what sources can you look at / involve with etc etc, it does rather shine a light on the importance of being cognisant of not just ‘where one is’ (eg, in a flat, in a tower block, in the suburbs of London) but how one can bring maximal resources to bear to help your own situation.
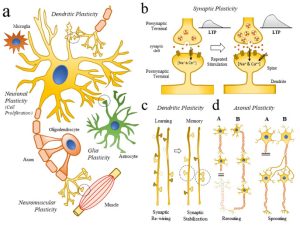 Your brain attempts to repair as much as possible after stroke, but there is a downside. During this period of repair, the neurons that surround the infarct are not able to do their job of conducting impulses.
Your brain attempts to repair as much as possible after stroke, but there is a downside. During this period of repair, the neurons that surround the infarct are not able to do their job of conducting impulses. The more a road is used or the more popular it may become (ie, if a new short-cut to a motorway has just been loaded to the sat-nav technology), the more traffic may build suddenly up along that route, so the council may strengthen the existing road to cope with the traffic and/or add more lanes or new routes to cope with the increased traffic (new connections). It will also add speed-bumps no doubt!
The more a road is used or the more popular it may become (ie, if a new short-cut to a motorway has just been loaded to the sat-nav technology), the more traffic may build suddenly up along that route, so the council may strengthen the existing road to cope with the traffic and/or add more lanes or new routes to cope with the increased traffic (new connections). It will also add speed-bumps no doubt!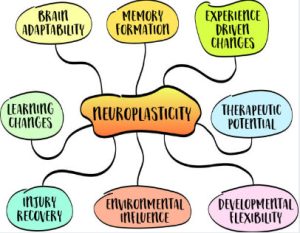 Neuroplasticity allows us to compensate for irreparably damaged neural pathways by strengthening or re-routing remaining ones. The more you use these pathways, your brain will respond by upgrading them so that they’re more efficient at handling the traffic and the quicker the information is sent. The more the pathways (or ‘roads’) are used, the more adequately functional a task, ability or skill may seem to become.
Neuroplasticity allows us to compensate for irreparably damaged neural pathways by strengthening or re-routing remaining ones. The more you use these pathways, your brain will respond by upgrading them so that they’re more efficient at handling the traffic and the quicker the information is sent. The more the pathways (or ‘roads’) are used, the more adequately functional a task, ability or skill may seem to become. A big secret to success with your upper limb for example (dependent on presentation) is, after early intensive recovery efforts have moved you to a certain standard of functional movement, to start ‘creating’ things with the thought of ‘formal rehab’ firmly in the background.
A big secret to success with your upper limb for example (dependent on presentation) is, after early intensive recovery efforts have moved you to a certain standard of functional movement, to start ‘creating’ things with the thought of ‘formal rehab’ firmly in the background. And furthermore, motivation must ‘run like a ribbon’ through the creative process. This must be intrinsic to the creator – there must be a NEED to create, to problem-solve until an objective is complete. This need stokes interest, drive, enthusiasm, desire, perseverance, passion and persistence.
And furthermore, motivation must ‘run like a ribbon’ through the creative process. This must be intrinsic to the creator – there must be a NEED to create, to problem-solve until an objective is complete. This need stokes interest, drive, enthusiasm, desire, perseverance, passion and persistence.
 Dr Tom Balchin, who founded the Action for Rehabilitation from Neurological Injury (ARNI) Charity nearly 25 years ago, has been made an Officer of the British Empire (OBE) in the New Year’s Honours List.
Dr Tom Balchin, who founded the Action for Rehabilitation from Neurological Injury (ARNI) Charity nearly 25 years ago, has been made an Officer of the British Empire (OBE) in the New Year’s Honours List.  To do this required Dr Tom create what has become the only existing national accredited qualification in rehabilitation after stroke for specialist personal trainers and therapists.
To do this required Dr Tom create what has become the only existing national accredited qualification in rehabilitation after stroke for specialist personal trainers and therapists.

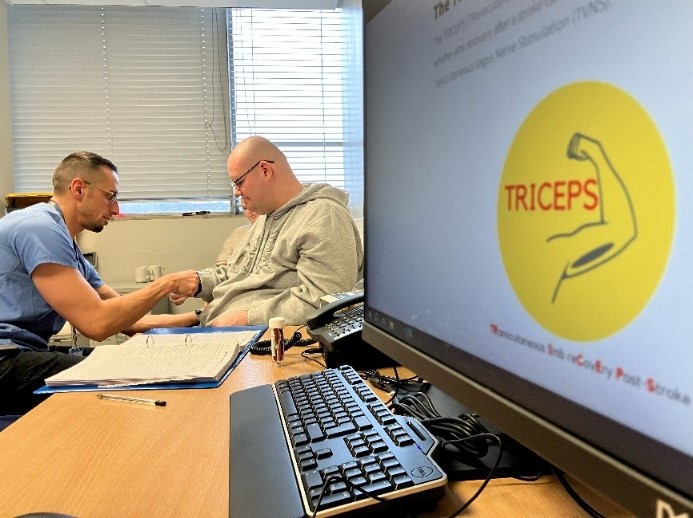

 Sheffield Teaching Hospitals and NHS Trusts nationally are looking for stroke survivors (aged 18+) with persistent arm weakness following an ischaemic stroke, which occurred between 6 months and 10 years ago.
Sheffield Teaching Hospitals and NHS Trusts nationally are looking for stroke survivors (aged 18+) with persistent arm weakness following an ischaemic stroke, which occurred between 6 months and 10 years ago.  I am interested, where can I take part?
I am interested, where can I take part?






 Are between 40-80 years of age.
Are between 40-80 years of age.
 ANDREW (BY MARION). September 2024.
ANDREW (BY MARION). September 2024.
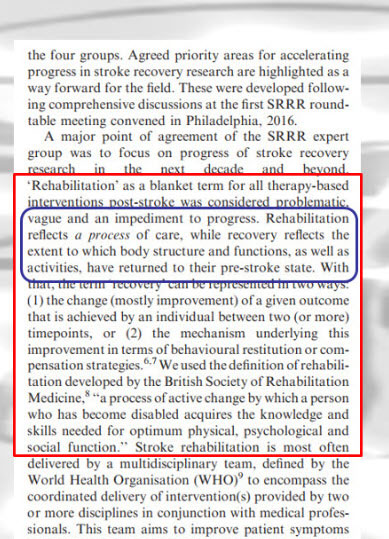
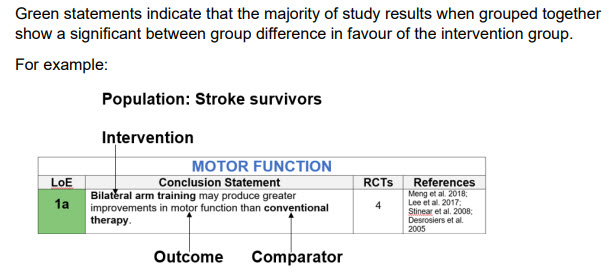

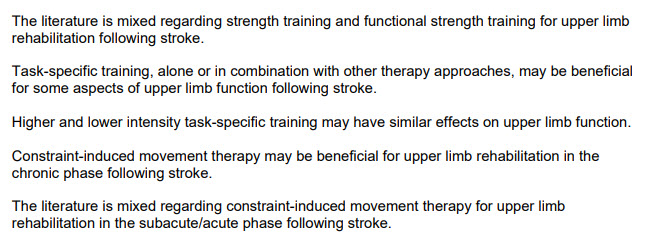
 The ‘sum of the evidence-base’ is the best we have to work with – it’s often a little out of date due to many factors, not least the nature of the time it takes to collate and display. But it’s being updated all the time. Also (I’ve found), there are very many very friendly experts in Universities who may certainly be approached in the right manner with a question or two, who will be able to refer you to online resources that may be appropriate to aid your further understanding. Ask me, if you like, and I may be able to help by asking a colleague researching in the area of your question.
The ‘sum of the evidence-base’ is the best we have to work with – it’s often a little out of date due to many factors, not least the nature of the time it takes to collate and display. But it’s being updated all the time. Also (I’ve found), there are very many very friendly experts in Universities who may certainly be approached in the right manner with a question or two, who will be able to refer you to online resources that may be appropriate to aid your further understanding. Ask me, if you like, and I may be able to help by asking a colleague researching in the area of your question. In short, as above, you need to try and understand the parameters of what you’re dealing with. This is something for when you’re now home or in other accommodation, such as your circumstances dictate.
In short, as above, you need to try and understand the parameters of what you’re dealing with. This is something for when you’re now home or in other accommodation, such as your circumstances dictate.
 Each year there are more than 100,000 first-time strokes in the UK; and as you may have heard on the news a couple of weeks ago, this number is set to rise by 50% by 2035.
Each year there are more than 100,000 first-time strokes in the UK; and as you may have heard on the news a couple of weeks ago, this number is set to rise by 50% by 2035. 
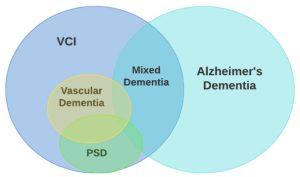
 struggling with memory issues, who may find music therapeutic and relaxing. It lets users play the piano, even if they haven’t played it in years (or ever), for free. With a library of thousands of songs, people with Alzheimer’s and dementia can use the app to access old favourite songs and unlock good memories in the process.
struggling with memory issues, who may find music therapeutic and relaxing. It lets users play the piano, even if they haven’t played it in years (or ever), for free. With a library of thousands of songs, people with Alzheimer’s and dementia can use the app to access old favourite songs and unlock good memories in the process.