 When people have strokes, loss of strength as a result can be extensive and a major contributor to prolonged recovery times. It’s estimated that the strength loss after the stroke is around 50% on the affected side of the body. The reasons for losing strength are related to factors such as weak neural activity after a brain injury and losing muscle mass (atrophy).
When people have strokes, loss of strength as a result can be extensive and a major contributor to prolonged recovery times. It’s estimated that the strength loss after the stroke is around 50% on the affected side of the body. The reasons for losing strength are related to factors such as weak neural activity after a brain injury and losing muscle mass (atrophy).
The evidence suggests that stroke survivors, at an appropriate time, should be guided to take part in some sort of regular resistance training that emphasises strengthening both affected and unaffected sides to prevent strength and muscle loss.
For example, one recent study, with 370 stroke survivors, showed that progressive resistance training had a large positive effect on strength regaining compared with no activity.

Structured resistance training can increase muscle mass (hypertrophy) and also has been shown to have positive effects on reducing anxiety, improving quality of life and cognitive function. Resistance training is often pretty simple to do, but does need guidance. It could be dynamic (moving an object such as a dumbbell for a few repetitions) or isometric (producing maximum contractions against static resistance), or a mixture of both.
Showing stroke survivors how to do simple targeted strength-training is a good thing, not only for managing the weakness caused by muscle-loss, but also for targeting spasticity (with limitations). Improving motor neuron recruitment by using gravity against limbs, weight of objects used in tasks, external support and external resistance are evidence-based parameters which can be manipulated to increase strength.
Furthermore, A recent Cochrane Review revealed that strong correlations exist in the current stroke rehabilitation research between improvements in strength and improvements in function. This is significant, as researchers previously did not have enough data not so long ago to make this evidence available for therapists and trainers to incorporate into their work with survivors.
 An invitation to you:
An invitation to you:
A group of researchers from Sheffield Hallam University, the University of Sussex and ARNI partnership are interested to know your thoughts on designing feasible home exercises for strengthening and mobilising the upper limbs after a stroke at a chronic stage (at least 6 months after stroke).
The research team recently secured a grant from UK Research and Innovation (UKRI) to investigate the methods to design smart and digital environments for stroke survivors at home (click the link below to the grant page to find out more).
What is this research about… and could it be of use to you to take part?
The research team are very interested in working with you, face to face, to find out your views about how best to create a digital programme to help improve muscle strength.
They would ask you to consider whether you would prefer to use forms of equipment such as weights, dumbbells, resistance bands and combinations of such items.

The research team would very much like to invite you to participate in a small group discussion (maximum 10 people) in a large boardroom at Lingfield Racecourse in Surrey, overlooking the race-track, with three researchers from Sheffield Hallam University and the University of Sussex, as well as Dr Tom Balchin and a number of the ARNI therapists to run the proceedings.
The object, as noted above, would be to share your opinions and experience in doing resistance training at home or in gyms. The session duration will be 2 hours with refreshments.

If you had a stroke at least in the last 6 months and you are ambulant (not a wheelchair user) and with experience in using fitness equipment (after or before your stroke), the team would be so grateful to to listen to your considered opinions…
Place, date and your travel fare paid.
The session is in person at Lingfield Park Marriott Hotel & Country Club (Lingfield, RH7 6PQ).
The date of this event in January 2023 is to be confirmed, but please enquire now.
You can choose to come either for 10.30-12.30 session or for the 13.30-15.30 session
The event is free and the Research budget will pay your travel fares up to £25.
Covid-19 Safety.
A message from the research team about Covid-19 safety: they will ask the participants and researchers to use a face mask and sit in a safe distance (2m). They will provide face masks and hand sanitisers and the windows in the room are open for ventilation. They will ask you to do not attend the session if you had any flu symptoms or you were with someone who was infected by COVID-19 in the last 10 days before the session.
Who to contact
If you like the sound of taking part in this study, please contact Dr Mohsen Shafizadeh (m.shafizadeh@shu.ac.uk) to register for this event or ask further questions. We will send you the Participant’s Information Sheet and other forms via email. You will sign a hard copy of the consent form in the session.
The Research team
Dr Mohsen Shafizadeh, Dr Khalid Ali, Dr Nasrin Nasr, Dr Tom Balchin, Dr John Hart, Dr John Kelley.



 For example, by the severity of your difficulties and perceived losses, your individual coping style, your familial/social support network, your cultural beliefs about disability, and your previous mental-health.
For example, by the severity of your difficulties and perceived losses, your individual coping style, your familial/social support network, your cultural beliefs about disability, and your previous mental-health. For example, it may be best to avoid crowds and stressful conditions, which may in turn make you feel overwhelmed. You can try learning relaxation techniques to help you combat any stress and fatigue you may experience after your stroke. There are lots of devices and apps to help you manage to bring emotions to an equilibrium over time.
For example, it may be best to avoid crowds and stressful conditions, which may in turn make you feel overwhelmed. You can try learning relaxation techniques to help you combat any stress and fatigue you may experience after your stroke. There are lots of devices and apps to help you manage to bring emotions to an equilibrium over time.
 Apathy can have negative impact on your recovery of function, your ADLs, general health, and quality of life. It can stop you from enjoying your social connections and bothering to do things that you enjoy. If you develop apathy, it can also lead to a significant extra burden for your families, carers and friends… and worries them because it’s obvious how it will hold you back from potentially conquering/coping better w the situation you’re in.
Apathy can have negative impact on your recovery of function, your ADLs, general health, and quality of life. It can stop you from enjoying your social connections and bothering to do things that you enjoy. If you develop apathy, it can also lead to a significant extra burden for your families, carers and friends… and worries them because it’s obvious how it will hold you back from potentially conquering/coping better w the situation you’re in. It can be easy to think that emotional changes will never improve, but research shows that you may well come to terms with the after-effects of your stroke, which may in turn help responses and mood to become more balanced.
It can be easy to think that emotional changes will never improve, but research shows that you may well come to terms with the after-effects of your stroke, which may in turn help responses and mood to become more balanced. These are most likely to be experienced by those working with families and carers working with survivors with significant cognitive, communication and physical difficulties. Behaviours can range in severity and most usually have a function such as communicating a frustrated or unmet need. Families and carers have to come to understand these behaviours as best as they can.
These are most likely to be experienced by those working with families and carers working with survivors with significant cognitive, communication and physical difficulties. Behaviours can range in severity and most usually have a function such as communicating a frustrated or unmet need. Families and carers have to come to understand these behaviours as best as they can. Consistent and positive support, such as that offered by an excellent therapist/trainer (a qualified ARNI Instructor being just one example) is a great way to start this, as such a person will come in to the home, offering an encouraging example of health and strength for the survivor to hopefully be motivated by, and will know many innovative strategies to trial with the person to help them be creative with their own recoveries.
Consistent and positive support, such as that offered by an excellent therapist/trainer (a qualified ARNI Instructor being just one example) is a great way to start this, as such a person will come in to the home, offering an encouraging example of health and strength for the survivor to hopefully be motivated by, and will know many innovative strategies to trial with the person to help them be creative with their own recoveries.
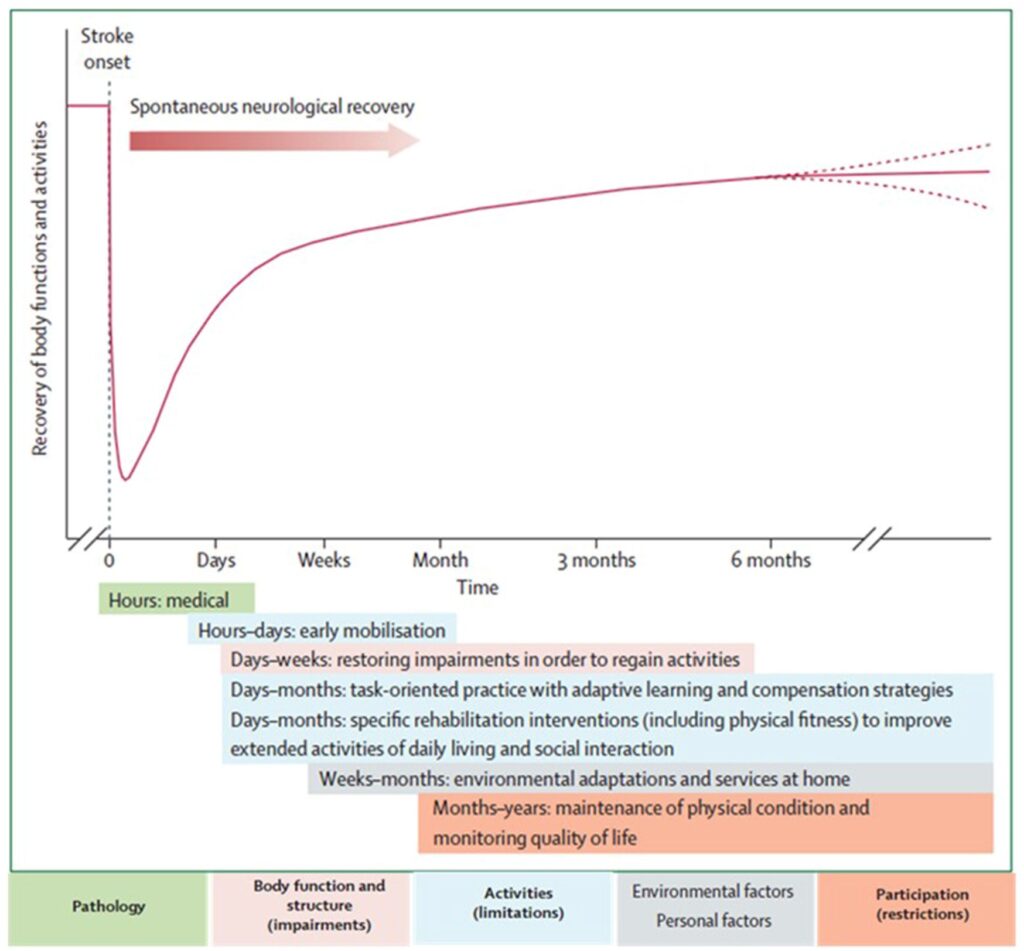 But you must also appreciate that a gradient of significant possible responsiveness to treatment (and also responsiveness to neglect of rehab/retraining) that extends after 12 months post-stroke has been uncovered, which is VERY relevant for the majority of stroke patients.
But you must also appreciate that a gradient of significant possible responsiveness to treatment (and also responsiveness to neglect of rehab/retraining) that extends after 12 months post-stroke has been uncovered, which is VERY relevant for the majority of stroke patients. To help with task-training, strength training and developing physical coping (not compensation) strategies, there are also so many adjuncts to community stroke rehab retraining these days – low tech to high tech – from AFO’s that can phase you on from rigid plastic orthotics, to upper limb de-weighting devices, simple and cost-effective devices like the
To help with task-training, strength training and developing physical coping (not compensation) strategies, there are also so many adjuncts to community stroke rehab retraining these days – low tech to high tech – from AFO’s that can phase you on from rigid plastic orthotics, to upper limb de-weighting devices, simple and cost-effective devices like the 





 Working with more than 100 therapists (occupational therapists and physiotherapists) and 200 stroke patients,
Working with more than 100 therapists (occupational therapists and physiotherapists) and 200 stroke patients, This platform includes a smartwatch app with tailored coaching to help people own their rehabilitation journey and inform their clinicians on their progress. The smartwatch app works like a step counter, it tracks minutes of arm activity through an algorithm developed for stroke survivors.
This platform includes a smartwatch app with tailored coaching to help people own their rehabilitation journey and inform their clinicians on their progress. The smartwatch app works like a step counter, it tracks minutes of arm activity through an algorithm developed for stroke survivors. This will involve wearing wrist-based sensors and motion trackers during a 2 hour session at Imperial’s White City Campus to carry out tasks of daily activities such as using a knife and fork, reading a book and more.
This will involve wearing wrist-based sensors and motion trackers during a 2 hour session at Imperial’s White City Campus to carry out tasks of daily activities such as using a knife and fork, reading a book and more.
 Please fill in this expression of interest form:
Please fill in this expression of interest form: 
 Rehabilitation after stroke is a partnership between you and your ARNI instructor or therapist. You’ll know that regular practice of techniques and exercises is necessary to optimise progress after stroke, but during the times that your Instructor isn’t present, these may or may not be difficult to perform.
Rehabilitation after stroke is a partnership between you and your ARNI instructor or therapist. You’ll know that regular practice of techniques and exercises is necessary to optimise progress after stroke, but during the times that your Instructor isn’t present, these may or may not be difficult to perform. Currently there is no stroke specific measurement tool available to do this. This study aims to address this gap in stroke rehabilitation.
Currently there is no stroke specific measurement tool available to do this. This study aims to address this gap in stroke rehabilitation.  If you have any questions, please contact Dylan Kerr (
If you have any questions, please contact Dylan Kerr (
 Tiredness is something we all experience in our everyday lives. But how about the sort of tiredness which seems to be unrelated to physical or mental exertion, and does not seem to be alleviated by rest? This is a real problem for many stroke survivors on top of the many other problems they may face – and is called ‘fatigue’.
Tiredness is something we all experience in our everyday lives. But how about the sort of tiredness which seems to be unrelated to physical or mental exertion, and does not seem to be alleviated by rest? This is a real problem for many stroke survivors on top of the many other problems they may face – and is called ‘fatigue’. The Effort Lab, led by
The Effort Lab, led by  It takes no more than 45 minutes on an online combined quiz and questionnaire:
It takes no more than 45 minutes on an online combined quiz and questionnaire: 
 Strong evidence exists that physiotherapy improves the ability of people to move and be independent after suffering a stroke. But at six months after stroke, we know that many people remain unable to produce the movement needed for every-day activities such as answering a telephone. So, what can be done?
Strong evidence exists that physiotherapy improves the ability of people to move and be independent after suffering a stroke. But at six months after stroke, we know that many people remain unable to produce the movement needed for every-day activities such as answering a telephone. So, what can be done? 2. Second, to optimise a physiotherapist’s chances to advise/work on an optimal combination of rehab interventions for each individual after stroke, it would be ideal to find out what kinds of sleep patterns are most beneficial for them.
2. Second, to optimise a physiotherapist’s chances to advise/work on an optimal combination of rehab interventions for each individual after stroke, it would be ideal to find out what kinds of sleep patterns are most beneficial for them. Ideally, more portable equipment should also be able to be accessed by therapists, which would cost less and is designed for use in small spaces. But such equipment would have to also be sensitive enough to provide meaningful feedback for therapists in a similar way to those used by the specialist labs. Such feedback could then be very useful for therapists and survivors to create optimal rehab plans together which would really enable the survivor to work on his/her edges of current ability.
Ideally, more portable equipment should also be able to be accessed by therapists, which would cost less and is designed for use in small spaces. But such equipment would have to also be sensitive enough to provide meaningful feedback for therapists in a similar way to those used by the specialist labs. Such feedback could then be very useful for therapists and survivors to create optimal rehab plans together which would really enable the survivor to work on his/her edges of current ability. A School of Health Sciences research team at the University of East Anglia (UEA) headed up by
A School of Health Sciences research team at the University of East Anglia (UEA) headed up by 
 Go for it if you can/if it’s appropriate for you!
Go for it if you can/if it’s appropriate for you!
 They’ll then place reflective markers on your skin. These markers are tracked by infra-red cameras placed at the top of the walls of the MoveExLab.
They’ll then place reflective markers on your skin. These markers are tracked by infra-red cameras placed at the top of the walls of the MoveExLab. 


 You can bet that I’ve met quite a few stroke survivors over the years who’ve become prone to anxiety, depression and/or
You can bet that I’ve met quite a few stroke survivors over the years who’ve become prone to anxiety, depression and/or  I hope that I’ve been able to facilitate at least some of these people towards the benefits of maintaining a ‘growth mindset’ concerning their recovery, despite their difficulties.
I hope that I’ve been able to facilitate at least some of these people towards the benefits of maintaining a ‘growth mindset’ concerning their recovery, despite their difficulties.
 Do MORE than able bodied people training-wise. Show them up!! Make them wish they WERE YOU!!
Do MORE than able bodied people training-wise. Show them up!! Make them wish they WERE YOU!!
 Accredited by ARNI Institute, Middlesex University and very kindly assisted by the Institute of Neurology, UCL, and other experts in neurorehabilitation including from Oxford University. The Course has run 3 times per year for 15 years.
Accredited by ARNI Institute, Middlesex University and very kindly assisted by the Institute of Neurology, UCL, and other experts in neurorehabilitation including from Oxford University. The Course has run 3 times per year for 15 years. All dates are 10.15am – 5pm on Saturdays, for easiest access.
All dates are 10.15am – 5pm on Saturdays, for easiest access. Please enquire.
Please enquire. 

