Hyun, J., Kim, J., Wang, S. et al. (2026). Magnetogel for minimally invasive occlusion of the left atrial appendage. Nature, 639, 94–101.
ONE MILLION POUNDS COMPENSATION FROM NHS FOR STROKE SURVIVOR
Wearable Robotics for Stroke Survivors and the Mechanics of Hip Assistance
The mechanical implementation of the 5.5-pound hip exoskeleton represents a quite innovative shift in wearable robotics, as it addresses the metabolic inefficiencies associated with hemiparetic gait. Developed at the University of Utah within the HGN Lab for Bionic Engineering, this research was spearheaded by principal investigator Associate Professor Tommaso Lenzi and lead author Kai Pruyn. The clinical findings, published in the journal Nature Medicine in October 2024, establish a new precedent for portable assistive technology. While previous attempts at stroke-specific robotics focused heavily on correcting foot drop via ankle-based systems, these often failed to reduce the physiological effort of walking because patients frequently compensate for distal weakness by over-recruiting proximal hip musculature. By targeting the hip joints directly, this device places the mechanical workload closer to the user’s centre of mass, allowing for lower torque requirements and a significantly lighter battery-powered motors system compared to cumbersome ankle-driven alternatives.
The trial utilised rigorous motion-capture techniques and instrumented treadmills to analyse the biomechanics of seven participants with hemiparesis. Data indicated that the intelligent control system, which synchronises with the user’s gait to provide a boost during hip flexion and extension, offloaded approximately 30 per cent of the biological work from the hip joints. This mechanical assistance resulted in an 18 per cent reduction in the metabolic cost of walking, a figure that provides a substantial relief equivalent to a healthy individual removing a 30-pound backpack. Such an improvement is critical because post-stroke fatigue often stems from the excessive caloric expenditure required to initiate and maintain a paretic step. Furthermore, the real-time customisation of assistance levels on each side allows for a symmetrical gait pattern, which is a primary goal in neurorehabilitation.
Beyond the immediate energy savings, the qualitative results from study participants like stroke survivor Lidia suggest that the device may facilitate secondary neuroplastic benefits. Her observations indicated that consistent use of the exoskeleton appeared to improve her unassisted movement, suggesting that the ‘boost’ provided by the robotic thighs helps the brain re-learn the correct timing of muscular engagement. This synergy between wearable engineering and biological recovery represents a sophisticated advancement in the treatment of one of healthcare’s biggest unmet challenges. The success of this hip-centric approach, following the lab’s previous acclaim for the Utah Bionic Leg, reinforces the potential for wearable robotics to transition from laboratory experiments to functional tools for daily living.
Although this technology has demonstrated life-changing potential in a laboratory environment, it’s not yet available for stroke survivors in the UK to buy. The research team at the University of Utah is currently partnering with leaders in the prosthetics and orthotics industry to transform the prototype into a commercial product, a process that involves extensive safety testing for home environments and the acquisition of necessary medical regulatory approvals.
L0BERAMISAL in Ischaemic Stroke Management
Addressing the long-standing clinical challenge of protecting the penumbra from secondary metabolic collapse, L0beramisal is a novel, intravenous dual-target neuroprotective agent developed by NeuroDawn Pharmaceutical for treating acute ischaemic stroke (AIS). It works by inhibiting the PSD-95–nNOS interaction and activating $\alpha$2-containing GABAAR to reduce brain injury.
Traditionally, neuroprotective strategies have failed in clinical trials due to their narrow focus on single pathways, such as glutamate excitotoxicity, but l0beramisal distinguishes itself by simultaneously modulating multiple cascades of neuronal death. Data presented at the 2026 International Stroke Conference by Dr Shuya Li confirms that this investigational therapy successfully shields vulnerable brain cells during the critical forty-eight-hour window following the initial vascular event. By utilising a dual-mechanism approach, the drug appears to stabilise the blood-brain barrier while concurrently inhibiting the oxidative stress and inflammatory responses that typically follow reperfusion. This multifunctional capacity is essential because the ischaemic cascade is a complex, multi-layered process where single-target interventions are often bypassed by redundant cellular pathways leading to apoptosis.
The Phase 3 clinical trial results indicate that the administration of l0beramisal intravenously for ten consecutive days leads to significantly superior functional outcomes when compared to a placebo. Participants who commenced treatment within forty-eight hours of symptom onset demonstrated higher scores on the modified Rankin Scale, suggesting a meaningful reduction in long-term disability and a higher degree of independent living. This ten-day intravenous protocol is designed to provide sustained support to neural tissues as they transition from the hyperacute stage of injury into the early phases of repair. Furthermore, the ability of l0beramisal to work in tandem with existing reperfusion strategies, such as mechanical thrombectomy and thrombolysis, suggests it may act as a vital adjunct that preserves tissue until blood flow is restored. This synergy is particularly important for patients who experience ‘reperfusion injury’, where the sudden return of oxygenated blood can paradoxically cause further damage to weakened neurons.
From a neurorehabilitation perspective, the stabilisation of neural tissue in the first two days post-stroke provides a more robust physiological foundation for subsequent recovery. ARNI Stroke Rehab UK emphasises that if more brain tissue is salvaged in the acute unit, the potential for successful neuroplasticity-driven training is vastly increased. When the primary motor cortex or descending corticospinal tracts are protected from secondary infarct expansion, survivors are better positioned to engage in high-repetition, task-specific exercises earlier in their journey. Therefore, loberamisal doesn’t ‘replace’ rehabilitation but rather enhances the substrate upon which physical therapy operates. The transition from acute neuroprotection to intensive, movement-based retraining is likely to become the new standard of care as these pharmacological advancements reach the bedside. If these results are standardised across stroke units, we may see a significant shift in the trajectory of recovery, moving away from managing permanent deficits toward a model of active neural preservation and functional restoration.
Functional Independence Via Paired Vagus Nerve Stimulation
The advancement of stroke rehabilitation continues to evolve with the integration of neuromodulatory technologies designed to augment traditional physiotherapy outcomes. A prominent development in this field is the TRICEPS trial, which was recently featured on the BBC Tech Now programme, featuring Dr Sheharyar Baig, a neurologist at Sheffield Teaching Hospitals NHS Foundation Trust. This clinical investigation focuses on the efficacy of Transcutaneous Vagus Nerve Stimulation (TVNS), a non-invasive method of stimulating the vagus nerve to facilitate neuroplasticity. Unlike earlier iterations of vagus nerve stimulation that necessitated the surgical implantation of a pulse generator, the TVNS approach utilised in the TRICEPS trial employs a specialised earpiece that delivers mild electrical impulses through the skin of the ear. This stimulation is specifically timed to occur during the performance of rehabilitation exercises, with the theoretical aim of “priming” the brain to be more responsive to motor retraining.
The underlying mechanism of paired vagus nerve stimulation involves the release of neuromodulators, such as acetylcholine and noradrenaline, which are critical for strengthening the neural connections required for motor control. By delivering these pulses while a survivor engages in task-specific exercises, the technology seeks to enhance the relevance of physical therapy and improve upper limb function. Clinical accounts from the trial, such as that of participant Amanda, illustrate the practical implications of this research. After six years of persistent right-hand impairment, Amanda reported significant functional gains following a 12-week regimen, which involved using the device for approximately one hour daily. These gains included the restoration of fine motor skills required for sewing and the ability to perform activities of daily living, such as dressing and housework, without assistance.
The TRICEPS trial is currently the largest study of its kind in the UK, operating across 19 NHS hospital sites, including the Royal Hallamshire Hospital in Sheffield. Following an independent review, the recruitment target has been expanded to 270 participants to ensure the statistical robustness of the final results. Eligibility is broad, including adults who have experienced an ischemic stroke between six months and ten years ago and who still suffer from moderate to severe arm weakness. As recruitment is scheduled to conclude in July, the trial organisers are actively seeking final participants to help establish whether this cost-effective, at-home solution can be scaled nationally. Interested survivors can apply through the Trial Manager, Kirsty McKendrick, or contact the team at triceps@sheffield.ac.uk.
5 Rarest & Most Bizarre Neurological Limitations After Stroke
While the majority of stroke survivors battle the well-documented hurdles of hemiparesis or aphasia, a small fraction of individuals find themselves navigating bizarre neurological landscapes that defy conventional understanding. One of the most striking is Alien Hand Syndrome, where a limb appears to act with a mind of its own, performing complex tasks like buttoning a shirt or grabbing objects without the person’s conscious intent. This dissociation between will and action is estimated to affect fewer than one per cent of stroke patients, yet for those involved, it creates a profound sense of physical betrayal. Because the condition is so rare and often misdiagnosed, only a handful of survivors ever receive the specialised sensory-motor training required to dampen these involuntary movements.
Equally disorientating is Alice in Wonderland Syndrome, a perceptual disorder where the survivor perceives parts of their own body or external objects as being wildly out of proportion. A hand might appear as large as a car, or the floor may seem to undulate like water, creating a terrifying lack of spatial stability. Research suggests this occurs in a very low percentage of cases, primarily when the stroke affects the parietal or occipital lobes. Despite the severity of the distortion, many patients are reluctant to seek help, fearing that their symptoms will be mistaken for psychiatric illness rather than a secondary effect of neural misfiring.
In some instances, the stroke can even alter a person’s perceived identity through Foreign Accent Syndrome. This occurs when damage to the speech centres of the brain changes the rhythm, pitch, and intonation of speech, causing the survivor to speak with a distinct accent they have never naturally possessed. While it is often treated as a media curiosity, it is a genuine clinical problem that affects roughly one in a thousand survivors. The psychological impact of losing one’s native voice is immense, yet specialised speech therapy designed specifically for this syndrome is incredibly difficult to access in the UK, leading to a low rate of successful intervention.
Even more elusive are Prosopagnosia and Cotard’s Delusion, both of which strike at the heart of human recognition and existence. Prosopagnosia, or face blindness, leaves a survivor unable to recognise the faces of their own family members or even their own reflection, despite their vision remaining perfectly clear. On the extreme end of the spectrum is Cotard’s Delusion, a nihilistic belief where the patient is convinced they have died, do not exist, or have lost their internal organs. These conditions are so exceptionally rare that they appear in fewer than 0.5 per cent of clinical cases. Consequently, the vast majority of those suffering do so in isolation, as standard rehabilitation units are rarely equipped to address these profound cognitive shifts.
Ultimately, these conditions represent the fringes of neurological recovery in 2026. While the chance of encountering them is statistically low, they are a daily reality for a resilient few who must find ways to cope with a world that has become unrecognisable. Because these problems are so rare, clinical data on successful management is scarce, making it vital for survivors to share their personal strategies. Do any of our readers suffer with these unusual limitations or perhaps something similarly rare?? If you have found a way to manage these unique challenges, please let us know in the comments below how you cope so that others might benefit from your experience!
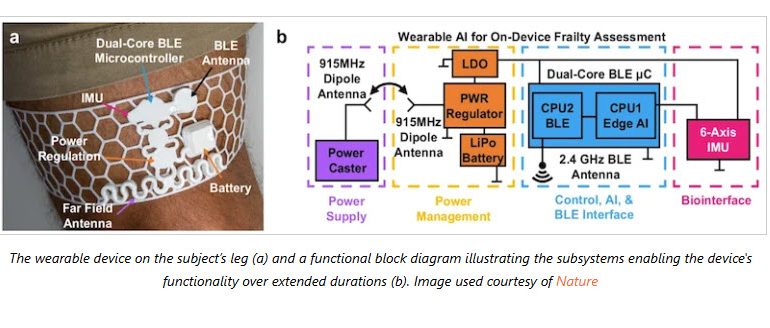
AI for Pre-emptive Frailty Diagnostics After Stroke
The clinical identification of frailty in the ageing population has historically been reactive, typically occurring only in the aftermath of a catastrophic event like a stroke, fall or other acute hospitalisation. To address this diagnostic lag, researchers at the University of Arizona have engineered an innovative wearable device designed to facilitate the early detection of frailty-related biomarkers through continuous physiological monitoring. This prototype, constructed as a lightweight 3D-printed mesh sleeve worn around the thigh, serves as a sophisticated biomechanical sensor suite. By focusing on the thigh, the device captures high-fidelity data regarding the primary muscle groups responsible for locomotion and balance, allowing for the precise measurement of acceleration, gait symmetry, and step variability. These metrics are critical, as subtle deviations in gait consistency often serve as the earliest indicators of physiological decline and increased fall risk long before clinical symptoms become overt to the patient or practitioner.
The technical architecture of the device distinguishes itself from conventional wearables through the integration of edge computing and artificial intelligence. Rather than transmitting raw, high-bandwidth data to a centralised server… a process that is often energy-intensive and raises privacy concerns… the device utilises an on-board artificial intelligence algorithm to synthesise and analyse the data in real time. This local processing capability reduces the volume of data transmission by approximately 99 per cent, transmitting only the summarised clinical insights to the healthcare provider. This efficiency not only extends the battery life of the wearable but also ensures that the summarized results are immediately actionable. Such a reduction in data latency is essential for preventative intervention strategies, as it allows clinicians to monitor the elderly population within their own domestic environments without the logistical burdens associated with continuous raw data streams.
Furthermore, the materials science involved in the development of the 3D-printed mesh ensures that the device is both durable and comfortable for long-term wear, which is a significant factor in patient compliance among the elderly. By quantifying frailty through objective longitudinal data rather than intermittent subjective assessments, this technology promises to transform the current geriatric care model into a proactive framework. The ability to observe fluctuations in gait symmetry and acceleration over weeks or months provides a granular view of a stroke survivor’s functional trajectory. This paradigm shift towards point-of-care diagnostics enables the implementation of targeted physical therapies or nutritional interventions at the earliest sign of frailty, effectively mitigating the risk of debilitating incidents and improving the overall quality of life for the ageing population.
Belfast VR Pilot Study Reveals 500% Increase in Movement Repetitions
Immersive tech is beginning to address the well-known challenge of therapeutic dosage. It’s widely recognised within the field of neuroplasticity that the restoration of motor function following a cerebrovascular accident is heavily dependent upon high-repetition, task-specific training. However, traditional occupational therapy often struggles to facilitate the volume of movement necessary to trigger cortical reorganisation, frequently limited by patient fatigue, time constraints, and the inherent monotony of repetitive exercises. The recent collaborative pilot study conducted by the Belfast Health and Social Care Trust, in partnership with the medtech firm eXRt, has provided compelling empirical evidence that virtual reality (VR) can bridge this gap. By trialling the Resynk platform, researchers have demonstrated that integrating digital immersion into standard care pathways can increase upper limb movement repetitions by as much as 500 per cent compared to conventional methods.
The technical efficacy of the Resynk platform lies in its ability to translate standard physiological movements into interactive, arcade-style feedback loops that bypass the psychological barriers to repetition. During the six-month longitudinal pilot, stroke survivors were subjected to a hybrid regimen consisting of both traditional occupational therapy and gamified VR sessions. The primary objective was to quantify the disparity in movement volume and evaluate the qualitative impact on patient engagement. The results were statistically profound; the immersive nature of the VR environment provided a continuous stream of visual and auditory stimuli that maintained the participants’ attention and drive. This engagement resulted in a surge of physical output, with one notable case study recording nearly 800 reps in a single thirty-minute session; a volume that is pretty much unattainable through standard manual therapy alone.
Furthermore, the study highlighted the critical importance of portability and environmental flexibility in modern neuro-rehabilitation. The Resynk system was designed to be utilised in various clinical settings, including at the patient’s bedside, in a seated position, or within a dedicated rehabilitation suite. This flexibility is essential for acute and sub-acute stroke survivors whose mobility may be restricted, allowing for the immediate commencement of high-intensity training. By facilitating such a massive increase in movement volume, the platform aligns with the latest clinical guidelines which advocate for more intensive therapy to maximise functional independence. The success of the Belfast trial suggests that stroke recovery in the UK will increasingly rely on these sophisticated digital interventions to supplement manual therapy and ensure that survivors reach the critical threshold of repetition required for meaningful neurological recovery.
Leading UK Stroke Research NO DM199 in Acute Neuroprotection
The clinical investigation of DM199, a recombinant human tissue kallikrein-1 (KLK1), represents a sophisticated pharmacological approach to the management of acute ischaemic stroke by targeting the microcirculatory environment of the brain. The University Hospitals of North Midlands NHS Trust (UHNM) has marked a significant milestone in British neuro-vascular research by recruiting the UK’s first patient into the ReMEDy2 global study at the Royal Stoke University Hospital. This phase 2/3 trial evaluates the therapeutic potential of DM199, which is designed to replenish the endogenous KLK1 protein that is often depleted during and after a stroke event. KLK1 plays a critical role in the regulation of local blood flow and the inflammatory response; by administering a recombinant version, researchers aim to promote vasodilation and enhance collateral circulation to the penumbra—the salvageable brain tissue surrounding the core of the infarct.
The pharmacological profile of DM199 is distinct from traditional thrombolytic agents, as it focuses on supporting the physiological mechanisms that naturally protect neural tissue rather than solely focusing on clot dissolution. In the context of an acute ischaemic event, the restoration of microvascular perfusion is essential to prevent the secondary cascade of neuronal death. The ReMEDy2 trial specifically targets patients who are not candidates for mechanical thrombectomy or those who have already received standard-of-care treatments but remain at risk of significant disability. By utilising the expertise of the North Midlands Clinical Research Delivery Centre (CRDC) in collaboration with the UHNM stroke service and research teams, the study seeks to determine if DM199 can significantly reduce the neurological deficit and improve long-term functional independence in stroke survivors.
This international collaboration is particularly vital because current treatments for acute ischaemic stroke are strictly limited by narrow therapeutic windows. The introduction of DM199 into the UK clinical landscape through the Royal Stoke University Hospital provides a unique opportunity to evaluate a therapy that may extend or complement existing protocols. Beyond the immediate vascular effects, DM199 is theorised to exert neuroprotective benefits by modulating the immune response and reducing the detrimental effects of reperfusion injury. As the ReMEDy2 study progresses, the data collected from the North Midlands site will contribute to a global understanding of whether this recombinant protein can redefine the standard of care for acute stroke patients worldwide. The integration of such high-level research into the NHS infrastructure ensures that UK survivors remain at the forefront of access to emerging biotechnological interventions.
Optimal Stroke Recovery Integrates Cognitive Training & Physical Re-training
Pioneering research led by a team from the Medical University of South Carolina, including Dr Stephanie Aghamoosa and Dr Michelle Woodbury, is currently proving that the mind and body must be trained as a single, cohesive unit to achieve true recovery. Their study, recently published in Brain Sciences and funded by the NIH, introduces the sophisticated COG-OT framework which integrates cognitive treatment directly with occupational therapy. This dual-track approach ensures that survivors do not simply work on physical movement in isolation but simultaneously build the essential mental foundations, such as sustained attention and executive function, required to drive meaningful motor learning during the most volatile stages of rehabilitation. By recognising that physical action is inextricably linked to cognitive processing, this research moves us beyond traditional, fragmented therapy models toward a more holistic understanding of how the brain relearns complex tasks.
This sophisticated model of care aligns perfectly with the overarching mission of the ARNI Stroke Rehab UK Institute, which has long championed the necessity of a multidisciplinary mindset for long-term success. While the ARNI Charity focuses on providing the elite physical strategies and task-specific practice needed for functional independence, there is a clear recognition that a survivor’s cognitive readiness is often the primary engine that powers their physical progress. By combining cognitive resilience with rigorous physical drills, it is possible to ensure that the brain is not only capable of learning new movements but is also robust enough to sustain the intense focus required for neuroplasticity to occur. This synergy between mental clarity and physical effort is what allows a survivor to transition from basic clinical movements to the fluid, autonomous actions required for daily life.
For the serious survivor, the vital takeaway is that this research validates the idea that recovery is a high-performance endeavour where every mental and physical variable must be optimised. The COG-OT approach suggests that by addressing cognitive barriers alongside physical ones, we can move away from a one-size-fits-all model and toward a far more precise and effective form of retraining. As Dr Balchin continues to integrate these evidence-based principles into the ARNI Approach, the goal remains to empower survivors to take full control of their journeys. Ensuring that mental clarity and physical strength work in perfect harmony is the most effective way to reclaim a life of autonomy, ensuring that the brain and body are equally prepared for the relentless pursuit of purpose.