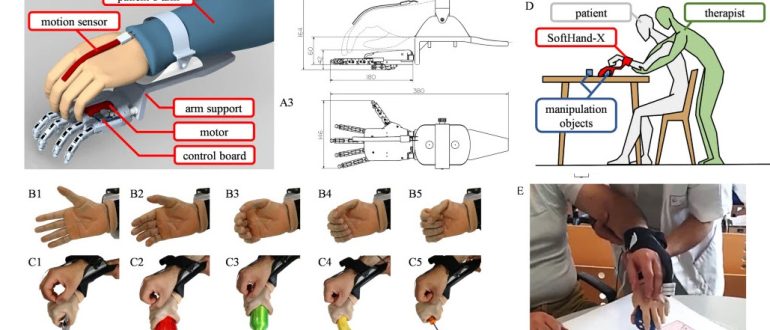
The RELab tenoexo 2.0 is an updated version of a wearable soft robotic hand orthosis designed to provide grasping assistance and support for rehabilitation in individuals with sensorimotor hand impairments, such as those following a stroke. This improved design features enhanced finger and actuation systems for greater simplicity and robustness, aiming to increase user independence and quality of life by facilitating high-dose, task-specific training in both clinic and home environments.
The latest findings on the RELab tenoexo 2.0 are of significant interest for our stroke rehabilitation community. A feasibility study just published in the Journal of NeuroEngineering and Rehabilitation demonstrates how this innovative, wearable device can significantly enhance hand and arm function for stroke survivors.
Researchers evaluated its effectiveness through a two-phase study involving individuals with chronic stroke. The survivors who used it achieved an impressive number of high-intensity repetitions, logging over 150 supported grasps per hour at home—a rate nearly five times higher than conventional therapy.
The intervention led to clinically meaningful functional gains in upper limb function, as measured by standardised tests like the Action Research Arm Test (ARAT) and Fugl-Meyer Assessment (FMA-UE). The functional gains observed were retained even one month after the intervention period ended, highlighting the therapy’s lasting impact. The study showed strong user acceptance and high adherence rates for both in-clinic and at-home training, proving its viability for continuous care.
For stroke survivors facing long-term hand impairments, accessing high-intensity, repetitive therapy is often a major challenge. The RELab tenoexo 2.0 clearly offers a useful addition to retraining solution as it’s a portable, easy-to-use tool. This approach can empower survivors to take control of their own recoveries, helping to promote neuroplasticity and improve independence in daily activities.
It looks to us at ARNI Stroke Rehab UK that wearable soft robotics are not just futuristic concepts; they are becoming a really useful augment to neurorehab.