A new national campaign, ‘Every Second Counts,’ launched recently by the HSE in Ireland, is driving home a vital message: the moment you suspect a stroke is the moment you dial 999 or 112. Developed with the invaluable support of stroke survivors and community groups, this campaign aims to close the gap between symptom awareness and swift action.
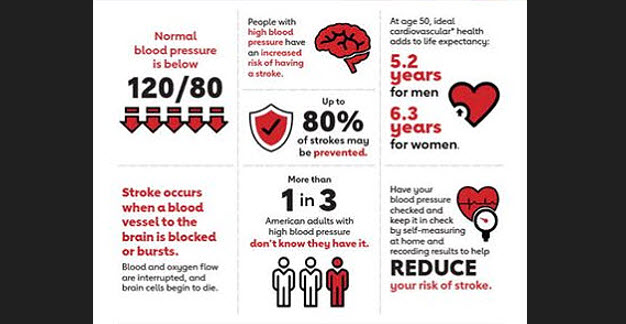
In Ireland, the statistics are sobering; every year, approximately 7,500 people experience a stroke and over 90,000 people are living with the resulting disability. Stroke is a leading cause of acquired neurological disability in Ireland and the third leading cause of death. Despite these figures, a concerning number of patients (fewer than 50%) arrive at the hospital within three hours of symptom onset. This is a critical window for life-saving and disability-reducing treatments.
Professor Rónán Collins, HSE National Clinical Lead for Stroke, emphasises that ‘every second counts’. He notes that while public awareness of the F.A.S.T. symptoms has improved, hesitation before calling an ambulance remains a significant issue. The new campaign is designed to overcome this hesitation and ensure that immediate action is taken.
Siobhán McGrath, a 34-year-old stroke survivor, understands the importance of immediate action first-hand. As a former Dublin senior ladies’ football team player, she initially didn’t recognise the signs of her own stroke three years ago and waited before seeking help. She now knows that this delay impacted her recovery and is a passionate advocate for the campaign.
Beyond raising public awareness, the National Stroke Strategy is also making significant progress in early stroke rehabilitation. A new report, Early Supported Discharge (ESD) for Stroke 2022 to 2023, highlights the success of a program that allows stroke survivors to receive therapy, social work, and nursing support at home.
The ESD model enables survivors to leave the hospital sooner and begin their recovery in the comfort of their own homes. This not only promotes greater independence but also improves bed capacity in hospital stroke units. In 2023, over 800 people benefited from ESD, a substantial increase from 2019. The expansion of ESD teams across Ireland is a key component of the National Stroke Strategy’s commitment to delivering more care in people’s homes.
Fine Gael politician & Minister for Health, Jennifer Carroll MacNeill, underscores the severity of stroke as a medical emergency and highlights the importance of quick treatment. With stroke incidence projected to rise in the coming decades, the Irish government is investing significantly in both public awareness and expanded services. This investment is aimed at ensuring more people can not only live longer after a stroke but also live to their full potential.