A recent £1.9 million investment by the Scottish Government is set to enhance stroke aftercare through the deployment of mobile heart-rate monitoring technology. This initiative, delivered via the Accelerated National Innovation Adoption (ANIA) pathway, aims to provide advanced diagnostic tools to approximately 8,000 stroke patients annually. The goal is to improve the detection of cardiac rhythm irregularities, particularly atrial fibrillation (AF), which is a significant risk factor for secondary stroke events.
The new technology involves ambulatory electrocardiogram (ECG) patch monitors. These compact, wireless and water-resistant patches are worn on the chest for up to 14 days and are designed to replace older, more cumbersome heart monitoring systems.
Clinical studies have indicated these patches are significantly more effective at detecting AF than previous methods, potentially reducing diagnosis and treatment times from several months to a few weeks. By facilitating a faster diagnosis of AF, clinicians can initiate preventative treatments more promptly, thereby reducing the patient’s risk of a recurrent stroke.
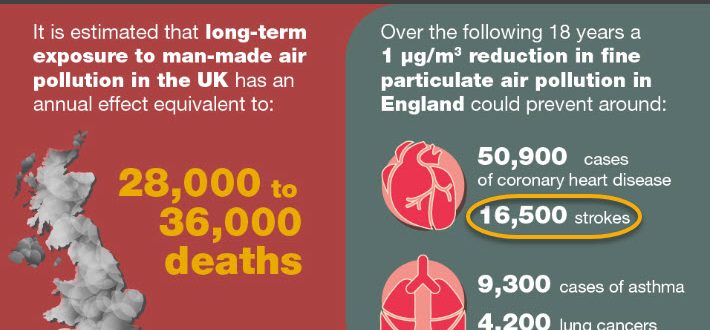
The projected outcomes of this investment are substantial. Over the next five years, it is estimated that the widespread use of these monitors could prevent nearly 700 secondary strokes and save more than 300 lives across Scotland. Beyond the clinical benefits, the initiative offers several operational and patient-focused advantages. By enabling at-home monitoring, it reduces the need for multiple hospital visits, improving patient convenience and reducing travel-related burdens.
The adoption of this technology is also expected to increase the efficiency of NHS Scotland by freeing up clinical capacity, including the equivalent of 15.7 full-time cardiac physiologists. Furthermore, the projected cost-savings for the NHS over the five-year period are estimated to be £14.6 million.
Overall, this investment represents a strategic application of innovative technology to improve patient care pathways for stroke survivors. It focuses on early and accurate detection to mitigate the risk of secondary events while simultaneously improving patient experience and operational efficiency within the healthcare system.