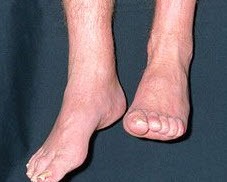
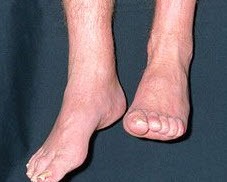
 Drop (or dropped) foot is common after stroke. Every stroke is different, and so are its side effects. Some stroke survivors may face different types of paralysis and others might only deal with a slight speech impairment. Either way, all stroke survivors should be aware of the possible side effects of stroke, and foot drop is one of them.
Drop (or dropped) foot is common after stroke. Every stroke is different, and so are its side effects. Some stroke survivors may face different types of paralysis and others might only deal with a slight speech impairment. Either way, all stroke survivors should be aware of the possible side effects of stroke, and foot drop is one of them.
This condition is related to high degrees of motor impairment, weakness or lack of voluntary control of your ankle dorsiflexors and increased spasticity of plantar flexors.
Foot drop interferes with the initial foot contact at the beginning of the stance phase and hinders ankle dorsiflexion during the swing phase of gait.
This changes the way you walk (it contributes to disruption in weight acceptance and weight transfer, reduces walking speed, efficiency and stability of gait), which in turn hinders your ability to complete everyday tasks and increases your risk of falls.
You may never recover completely from this very significant limitation, as with many effects resulting from stroke.
But it’s possible to learn, and create, some incredible combinations of strategies to manage this problem. An ARNI instructor can help you with this.
The severity of your condition will dictate your requirements, but if you have this difficulty, you may need an ankle-foot orthosis (AFO). This kind of splint lifts your toes and supports your ankle so that you can put your weight through your leg when you stand. It then prevents you from catching your toes when you walk. By the time you emerged from the hospital you may well have been wearing an ‘off-the-shelf’ one or a custom one produced by the orthotics department.

A rigid plastic AFOs is intended to keep you safe, and by and large, it will. It will help keep your foot in place so that you can move safely. But unfortunately, there’s some downsides to using an AFO. One known side-effect is that prolonged use can possibly guide you into ‘learned non-use’ of the muscular structures of lower leg after a while. This pattern of non-engagement occurs because you don’t have to work hard at a whole host of things such as maximal knee lift, actively engaging your hamstrings, beating circumduction, heel-striking, minimising ‘slappage gait’ and preventing ‘foot roll’.
However, an AFO may be the very best thing to help mobilise you. Wear one while you retrain, by the way, especially at first. For most, an AFO works in order to keep you safe if you have dropped foot, but the big secret to AFO is that you’ve got to actively minimise their use over time. This will help you slowly start to outgrow the need for one. Or outgrow the need for one which is quite so supportive.
How you’ll potentially regain independence and minimise the negative effects of foot drop, certainly insofar as to mobilise well?
 A Dr Tom solution (!) (for select survivors of course, but this can be ‘tweaked’ per survivor to end up as ‘big, generalisable concepts for most survivors), goes like this (and do ask a therapist or trainer to add to the below as they see fit):
A Dr Tom solution (!) (for select survivors of course, but this can be ‘tweaked’ per survivor to end up as ‘big, generalisable concepts for most survivors), goes like this (and do ask a therapist or trainer to add to the below as they see fit):
Re-training (repetitive walking practice plus appropriate strength training) PLUS a support/brace (as advised/applied by a therapist as appropriate AND how gradually to minimise their use if/as appropriate) PLUS techniques/strategies PLUS supportive footwear like neutral/under-pronator trainers and others.
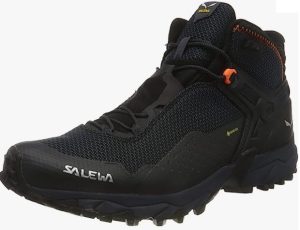
Trainers? Yes. Most people have NO idea how much of a difference supportive shoes/trainers make after stroke. If you have any questions, ask me and I’ll do my best to answer, refer to the evidence and/or ask an expert colleague.
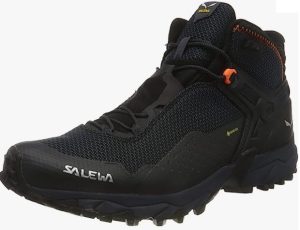
See my personal current ‘fave’: (I’ve had 3 pairs of these now: Salewa Trail Shoes ; they last for ages). Very expensive, yes, but these can make THE difference (although for a lady, they are hardly a delicate shoe!) for you. Experiment. These ones for instance seriously HELP with drop foot – and have Michelin Technical Performance soles, which is great. The ‘special rubber compound and design with selected grooves and studs ensures exceptional traction and stability on hard, uneven terrain’. Yes please.
The trick is that, as you put in the hard work and do more and more mobilisation, over time you might be able to graduate to a less obtrusive AFO brace or support.

You’ll need to buy and try these to work out which one suits you best. The best ones now are hinged and/or flexible. Some are made of carbon fibre. A new-to-the market support used by a number of my patients is the Turbomed FS3000 AFO.
Many survivors, over time, however want to find a very minimal and unobtrusive ‘stealth’ type of support, having worked out that the more minimal support they give to their foot, the harder they have to work in order to cope (which stimulates neuroplasticity massively). They may find a ‘figure-of-eight’ type support useful, with permission/advice/guidance from a therapist.

The ProMedics Lincoln Ankle Brace is a good example of one of such a support, and when I needed it, it worked for me too. I have residual dropped-foot so I know whereof I speak!
Btw, be careful if ordering/considering this particular brace/support, as the company have taken to pulling the strap as a seam from around the underside, rather negating its efficacy. Ask for the older version shown here (I’m fairly sure they can find old stock or just custom-make it for you).
Avoid any brace with a lumpy seam running along the bottom of it; this won’t be fun to walk on for long periods during the day. A tip is to wear a close-fitting sock between your skin and the brace or support to ensure comfort and help prevent rubbing.
Another support which works well is a Silicone Ankle Foot Orthotic. The Ottobok SAFO is a good example. A SAFO supports your foot not from below, but across the arch of the foot from above, in order to prevent the foot from dropping. The advantage of this principle is that because of the thin, flexible sole, you can feel the ground conditions directly and detect uneven surfaces such as stones and doorsteps. The result can be enhanced safety and self-confidence when walking.
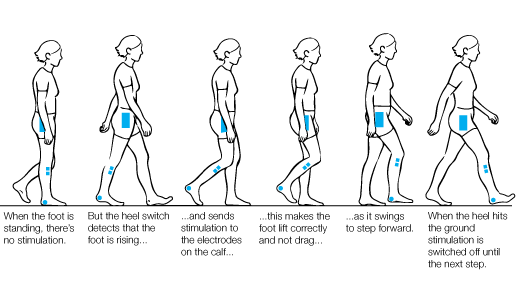
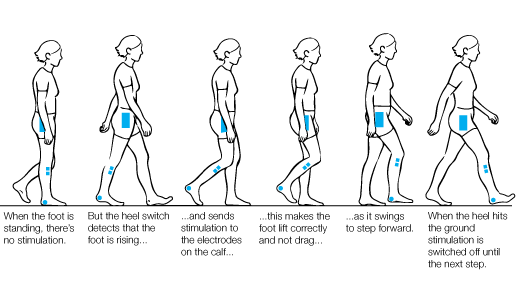
Functional Electrical Stimulation (FES) for drop foot management reveals consistently in the evidence to be more effective than using an AFO. It can improve ankle dorsiflexion, balance, and functional mobility, especially when combined with physiotherapy. But we don’t know what the results are for users over the long term as far as users becoming reliant on the FES technology.
It is known that FES devices that have been fitted correctly in a specialist centre can enable patients to learn to walk correctly and go some way to minimising muscle wastage. Implantable FES devices have been available for many years also.
PLEASE write below to help others who are considering using orthotics and/or FES for drop-foot. Or any other helpful suggestions you’ve found work well for you! Many thanks, Tom
 Your exclusive free invitation for 3 hours Conference on January 20th 2024:
Your exclusive free invitation for 3 hours Conference on January 20th 2024: 



 Virtual reality (VR) basically means interactive simulations of activities within environments that appear and feel similar to real-world objects and events (augmented reality).
Virtual reality (VR) basically means interactive simulations of activities within environments that appear and feel similar to real-world objects and events (augmented reality). VR interventions can be expensive but most are usually created to be affordable. A set-up often features just a keyboard, a mouse, a specialised multi-modal device such as a console or gloves with built-in movement sensors. Haptic devices are a good example of this. VR devices often provide feedback on movement execution and goal attainment. Many will help you to repetitively practice large and small movement-based tasks through the use of fun and motivating activities that can be completed while sitting, standing or lying.
VR interventions can be expensive but most are usually created to be affordable. A set-up often features just a keyboard, a mouse, a specialised multi-modal device such as a console or gloves with built-in movement sensors. Haptic devices are a good example of this. VR devices often provide feedback on movement execution and goal attainment. Many will help you to repetitively practice large and small movement-based tasks through the use of fun and motivating activities that can be completed while sitting, standing or lying. A
A 




 Another
Another  The analysis was limited in many ways: for example. the highest number of studies conducted to date have been in Asia, Europe, and North America, and no studies have been reported from Africa, South America, and Australia, so this problem adversely affected the generalisability of the study results. Nevertheless, the results of this large-scale meta-analysis show that, compared to the elderly who did not receive the flu vaccine,
The analysis was limited in many ways: for example. the highest number of studies conducted to date have been in Asia, Europe, and North America, and no studies have been reported from Africa, South America, and Australia, so this problem adversely affected the generalisability of the study results. Nevertheless, the results of this large-scale meta-analysis show that, compared to the elderly who did not receive the flu vaccine,

 The Department of Computing at Imperial College London is evaluating a platform called ‘CogiGames Home’, and have asked ARNI Charity to pass this message below to stroke survivors, carers (and professionals to forward if appropriate):
The Department of Computing at Imperial College London is evaluating a platform called ‘CogiGames Home’, and have asked ARNI Charity to pass this message below to stroke survivors, carers (and professionals to forward if appropriate): 




 Balance (both standing and walking) training is the only effective treatment for balance disorders, as recommended by the National Institute for Health and Care Excellence (NICE) UK
Balance (both standing and walking) training is the only effective treatment for balance disorders, as recommended by the National Institute for Health and Care Excellence (NICE) UK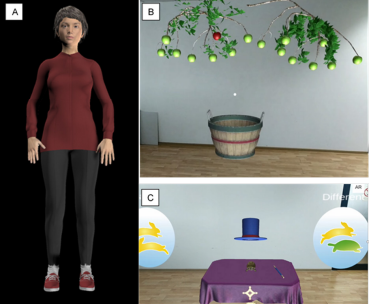 At University College London’s Institute of Neurology, a large-scale global research project (funded by a European Union Horizon 2021 grant), is under way (led by
At University College London’s Institute of Neurology, a large-scale global research project (funded by a European Union Horizon 2021 grant), is under way (led by 
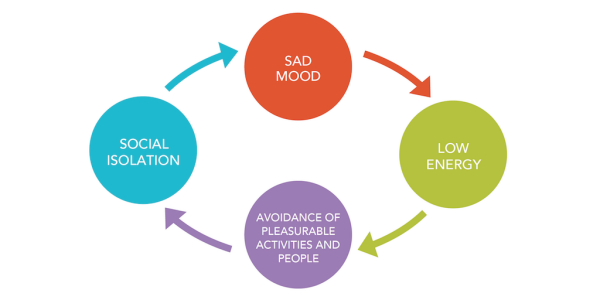

 Researchers from the Translational Neuropsychology Lab at the University of Oxford are interested in designing better treatments for depression in stroke survivors.
Researchers from the Translational Neuropsychology Lab at the University of Oxford are interested in designing better treatments for depression in stroke survivors. First, a member of the research team will contact you and see if you are eligible. This will involve them asking you some questions to make sure you are:
First, a member of the research team will contact you and see if you are eligible. This will involve them asking you some questions to make sure you are: For further help with this issue, please contact DEPRESSION ALLIANCE: A UK charity which helps people with depression, run by sufferers themselves.
For further help with this issue, please contact DEPRESSION ALLIANCE: A UK charity which helps people with depression, run by sufferers themselves. 
 The new (April 2023) stroke guidelines state (click link):
The new (April 2023) stroke guidelines state (click link):  However, access to specialist balance rehabilitation services can be poor due to the lack of enough specialists and sufficient health resources. Current programmes can be sub-optimal in that they are not truly multisensory, do not include any cognitive component (which is a key factor in determining both static and dynamic balance), and do not address real life symptoms reported by patients as challenging.
However, access to specialist balance rehabilitation services can be poor due to the lack of enough specialists and sufficient health resources. Current programmes can be sub-optimal in that they are not truly multisensory, do not include any cognitive component (which is a key factor in determining both static and dynamic balance), and do not address real life symptoms reported by patients as challenging.
 Research, led by
Research, led by 


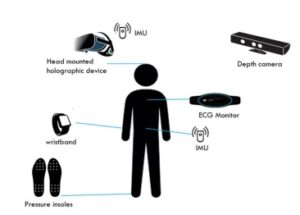 During the focus group, the team will have you watch a video which explains the HOLOBalance system. The team will then conduct semi-structured interviews related to the system usability and experience. They may also ask you additional questions as a group, to gather further feedback on the system.
During the focus group, the team will have you watch a video which explains the HOLOBalance system. The team will then conduct semi-structured interviews related to the system usability and experience. They may also ask you additional questions as a group, to gather further feedback on the system. 


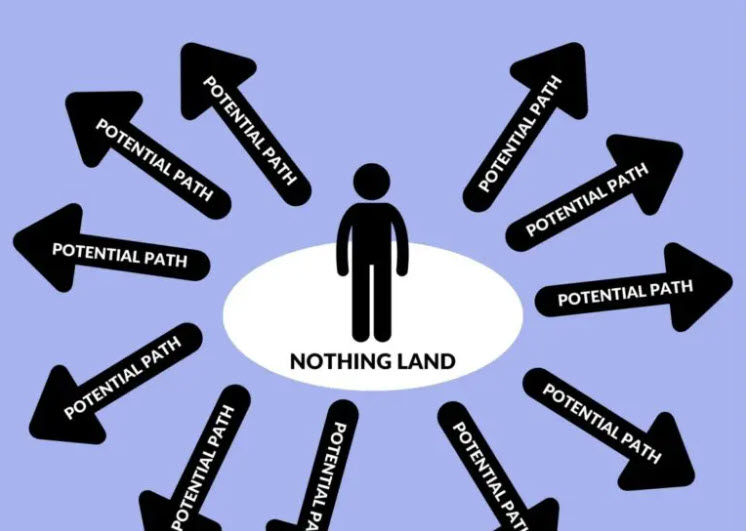 So many stroke survivors, at varying points during their respective times from stroke, have no idea how to start (or re-start) their recoveries. Or they do know about some options. But in either circumstance a majority don’t know what to do for themselves to stand the best chances of gaining some functional success for their efforts.
So many stroke survivors, at varying points during their respective times from stroke, have no idea how to start (or re-start) their recoveries. Or they do know about some options. But in either circumstance a majority don’t know what to do for themselves to stand the best chances of gaining some functional success for their efforts. 
 The reason why it’s important to be able to ‘contextualise/frame yourself’ in terms of the possible progress you can make by comparing yourself to existing data (seeing where you might fit or be one of those outliers etc), is that in the community, it’s very unlikely that you’ll be able to have any of the types of measures applied to you that therapists use clinically on patients unless one is working actively with a therapist.
The reason why it’s important to be able to ‘contextualise/frame yourself’ in terms of the possible progress you can make by comparing yourself to existing data (seeing where you might fit or be one of those outliers etc), is that in the community, it’s very unlikely that you’ll be able to have any of the types of measures applied to you that therapists use clinically on patients unless one is working actively with a therapist. For instance, if you love playing golf and really want to get back to it after stroke, it might not be appropriate to practise straightaway with your Number 5 iron in your house, unless you have a high ceiling and your control is already very good!
For instance, if you love playing golf and really want to get back to it after stroke, it might not be appropriate to practise straightaway with your Number 5 iron in your house, unless you have a high ceiling and your control is already very good! 
 Finding a Speech and Language therapist after discharge is notoriously difficult and SLTs are almost exclusively clinical and/or have big case-loads to take care of. And we know that SLT is often prohibitively expensive to engage with or just unaffordable, meaning people just get incredibly frustrated.
Finding a Speech and Language therapist after discharge is notoriously difficult and SLTs are almost exclusively clinical and/or have big case-loads to take care of. And we know that SLT is often prohibitively expensive to engage with or just unaffordable, meaning people just get incredibly frustrated.
 Storm Anderson, a UK-based speech and language therapist who has predominately treated adults affected by stroke and other acquired brain injury in acute hospital settings as well as out-patient and home-based settings. She has completed her BSc in Speech Language Pathology and MSc in Stroke Medicine, and is currently undertaking her PhD at Queen Square, UCL, using the PLORAS (Predicting Language Outcomes After Stroke) datasets.
Storm Anderson, a UK-based speech and language therapist who has predominately treated adults affected by stroke and other acquired brain injury in acute hospital settings as well as out-patient and home-based settings. She has completed her BSc in Speech Language Pathology and MSc in Stroke Medicine, and is currently undertaking her PhD at Queen Square, UCL, using the PLORAS (Predicting Language Outcomes After Stroke) datasets. Olivia Hodgkinson, a Johannesburg-based qualified Speech Language therapist who completed her BSc and MSc in Speech and Language Pathology at Cape Town University. She has substantial experience in both clinical (acute, sub-acute, specialised rehab and extended units) and educational settings. who has worked within highly diverse settings and within multidisciplinary teams and units. She has led and run therapy departments, supervised and mentored speech therapy university students, developed school based educational assessment programs and support structures for specialised learning units, initiated and implemented training for staff, allied professionals, family and caregivers on a variety of scope related topics in school, hospital and community based settings. She has strong dysphagia experience and skills and is a certified Vital-stim practitioner. She has a great passion for adult neurological injuries and disorders, voice disorders and dysphagia and is looking forward to helping you!
Olivia Hodgkinson, a Johannesburg-based qualified Speech Language therapist who completed her BSc and MSc in Speech and Language Pathology at Cape Town University. She has substantial experience in both clinical (acute, sub-acute, specialised rehab and extended units) and educational settings. who has worked within highly diverse settings and within multidisciplinary teams and units. She has led and run therapy departments, supervised and mentored speech therapy university students, developed school based educational assessment programs and support structures for specialised learning units, initiated and implemented training for staff, allied professionals, family and caregivers on a variety of scope related topics in school, hospital and community based settings. She has strong dysphagia experience and skills and is a certified Vital-stim practitioner. She has a great passion for adult neurological injuries and disorders, voice disorders and dysphagia and is looking forward to helping you!