So, what’s the point of task-specific practice and why should you do it? Can assistive devices help much? Are they ‘better’ than a therapist or trainer? Or is there very little point in employing them? What about in tandem?

You’ll probably know well that upper limb weakness is a common, disabling and persistent problem after stroke and is a major contributor to many survivors’ poor well-being and quality of life. Conventional upper limb rehabilitation has had limited success and novel combined interventions are being investigated in an effort to stimulate greater recovery.
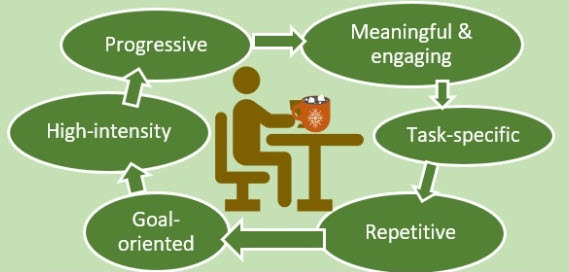
Although probably ever-under investigation for strong evidence of efficacy for stroke rehabilitation (!), task-specific practice can be said to be one of the best weapons stroke survivors have to try and engage plasticity. It also must not only reinforce recovery milestones, such as sitting balance, standing upright and the ability to walk but also tackle behaviours that are introduced after stroke, particularly with upper limb recovery.
A concern for many years amongst professionals in stroke has been (alongside what/when/how task-training can most effectively be done), the efficacy with which it may be augmented using devices ranging from active orthotics and robotics to medications.
My colleague, Sarah Valkenborghs in 2019, with the aid of her group, carried out a systematic review with a meta-analyses to find the evidence for combining assistive devices to task-specific training following stroke. From 3494 citations identified in 7 databases, 21 adjunctive interventions including electrical stimulation, transcranial magnetic stimulation, robotic devices, mental practice, action observation, trunk restraint and virtual reality were included. Only peripheral nerve stimulation with task-practice demonstrated small additional benefits over those of task-specific training alone for upper limb impairment. They concluded that there is little evidence that adding another intervention to task-practice confers additional benefits.
Rozevink at al, 2023 found, in a systematic review and meta-analysis analysing on the effectiveness of task-specific training using assistive devices and task-specific usual care on upper limb performance after stroke that task-specific training using assistive devices seems to be more effective in reducing impairment compared with task specific usual care in the subacute phase after stroke, but equally effective in the chronic phase of stroke.
 So, overall, whether using an assistive device or not when doing re-training, ‘task-practice’ is pretty much necessary/required.
So, overall, whether using an assistive device or not when doing re-training, ‘task-practice’ is pretty much necessary/required.
And for stroke survivors doing their best to recover in the community, it’s probably best to focus on task-training with a trainer or therapist, supplemented by lots of ‘retraining task-specific homework’ that any effective professional will be able to guide them into/support them with, and regard assistive devices (such as can be affordable), as useful adjuncts which can often facilitate task-training if/as as appropriate.
Dutch researchers (Kollen, Kwakkel & Lindeman) reported that ‘intensity and task-specific exercise therapy are important components of such an approach’. I have found that there is a strong case for implementing and balancing both into an Approach, with the addition of strength training. It’s what I did (and still do) to retrain, manage and ‘negate’ my own physical limitations. And it is how so many others are being taught how to get some significant results in terms of upper limb capacity AND performance (in ADLs).
 Task training is critical because it will ‘force’ you to practice using your more-affected limb. This is why the Evidence-Based Review of Stroke Rehabilitation (EBRSR) concludes that constraint induced movement therapy (CIMT) in clinical settings, for those who meet the qualifying criteria, shows strong evidence of benefit in comparison to traditional therapies in the chronic stage of stroke. CIMT is a great example of task training for the upper-limb. 30 to 66 % of stroke survivors report no longer being able to use the affected arm despite trying to rehabilitate and are in danger of avoiding using it (‘learned non-use’ or inattention/ neglect of the limb). Several factors might explain this phenomenon. First, you may see no reason to try and use your bad arm and therefore remain ignorant of underlying motor potential. Second, you may not know how to use any emerging isolated movement for functional performance.
Task training is critical because it will ‘force’ you to practice using your more-affected limb. This is why the Evidence-Based Review of Stroke Rehabilitation (EBRSR) concludes that constraint induced movement therapy (CIMT) in clinical settings, for those who meet the qualifying criteria, shows strong evidence of benefit in comparison to traditional therapies in the chronic stage of stroke. CIMT is a great example of task training for the upper-limb. 30 to 66 % of stroke survivors report no longer being able to use the affected arm despite trying to rehabilitate and are in danger of avoiding using it (‘learned non-use’ or inattention/ neglect of the limb). Several factors might explain this phenomenon. First, you may see no reason to try and use your bad arm and therefore remain ignorant of underlying motor potential. Second, you may not know how to use any emerging isolated movement for functional performance.
One more point: emerging minimal movement is often very overlooked. even if visible, it’s often considered non-functional. But this is very wrong. You actually need to try and regain an increase in active range of motion (AROM) in as many planes and pivots as possible. Increases in non-functional AROM increases strength and muscle bulk, encourages muscular activity which promotes vascular return, decreases the potential for soft-tissue shortening, and damage with resultant pain and stiffness – and increases osteoblastic activity on the affected and often osteoporetic) side.

So, try to do MORE with your more-affected upper limb by yourself each day (ie work towards a new goal, and check retention during your ADLs constantly afterwards (because you can lose ability, just like strength (which is shockingly easy to lose). Repeated attempts to use your affected limbs in training creates a form of practice that can potentially lead to further improvement in performance. The ideal is to find oneself in a ‘virtuous circle’, in which spontaneous limb use and motor performance will reinforce each other and re-teach your body to control the position of an affected limb.
In formal retraining situations it’s important to advance quickly toward practice of whole tasks with as much of ordinary environment context made available as possible. For example, say, a goal of yours is to improve the action control of your paretic foot for being able to cope whilst walking outside on the pavement, unsupervised and with no supports. The best retraining you can get is to ask a trainer or friend to plan a route for you to go with him or her, so that you can trial it safely and under careful supervision. You can work on leaving your stick and/or supports behind or using/wearing them according to your current levels of ability.
Many stroke survivors can be assisted to retrain by advising them to have one place and a set amount of times per week in which they devote time to their retraining. I tend to promote the importance of setting up a small matted ‘training area’ in your house, which needs only to be a few square metres wide. You also need a chair and a small table with a task-board, more advanced challenge board and other small items on it.
You need to finding your own task specifics, according to your goals. You also need to work on ‘close-simulations’. Even though simulations are probably not as effective for motor learning as performing the actual task, and remember, we are after significant performance improvement via task practice, you can see that this approach gives you some great advantages. It keeps you in the training area, keeps you working on-task and keeps you safe. And then outside of the training area, you need to make an effort to practice the tasks (or the components of them that you can manage), as part of your ADLs, noting changes when you can.
 One great example: I created ‘DJ-Therapy’ to get my upper limb working again. I basically made up a hugely successful paradigm which was suitable for me. How I did it is all listed in The Successful Stroke Survivor.
One great example: I created ‘DJ-Therapy’ to get my upper limb working again. I basically made up a hugely successful paradigm which was suitable for me. How I did it is all listed in The Successful Stroke Survivor.
You can read how I started it ‘off-decks’, then used the decks themselves to absolutely superb effect – ‘training’ 5 or so hours per day. It was never ‘training’ per se, for me, however.
Making training ‘not training’ is one of the biggest secrets to getting optimal success with upper limb function. I wish more people would have a go at this idea. Have a think about what might be suitable for YOU to keep YOU practising and interested.
Messages from this post are:
- Task-practice comes first and may not be significantly augmented by interventions: time to get busy, in other words.
- To start, get clued up to understand how to set up a training methodology
- An excellent starter for 10 is shown on these stroke rehab online videos (available for anytime login btw and half-price for a limited time).
- Get some help from a trainer or therapist to do task-practice,
- Perform as many specific, whole tasks of your choice inside a safe training area as you can.
- Work on the ‘edges of your current ability’.
- If the task is not appropriate to perform in your training area, you should try and to practise for it using close simulations in your training area first.
- Progress on task performance must consistently be checked outside your training area.
- If you can, you should try and pinpoint new action control in your ADLs to something you are doing in retraining.
- Make task-practice highly meaningful for you.
- And repeat! Many many many times. And have fun with it. Make things. Create.
- Investigate to see if you can find any appropriate technology for stroke rehab.
- Get assessed to see if any treatments, augments, devices or drugs are appropriate for you at your current (stage).
(2023) Effectiveness of task-specific training using assistive devices and task-specific usual care on upper limb performance after stroke: a systematic review and meta-analysis, Disability and Rehabilitation: Assistive Technology, 18:7, 1245-1258, DOI: 10.1080/17483107.2021.2001061






 Virtual reality (VR) basically means interactive simulations of activities within environments that appear and feel similar to real-world objects and events (augmented reality).
Virtual reality (VR) basically means interactive simulations of activities within environments that appear and feel similar to real-world objects and events (augmented reality). VR interventions can be expensive but most are usually created to be affordable. A set-up often features just a keyboard, a mouse, a specialised multi-modal device such as a console or gloves with built-in movement sensors. Haptic devices are a good example of this. VR devices often provide feedback on movement execution and goal attainment. Many will help you to repetitively practice large and small movement-based tasks through the use of fun and motivating activities that can be completed while sitting, standing or lying.
VR interventions can be expensive but most are usually created to be affordable. A set-up often features just a keyboard, a mouse, a specialised multi-modal device such as a console or gloves with built-in movement sensors. Haptic devices are a good example of this. VR devices often provide feedback on movement execution and goal attainment. Many will help you to repetitively practice large and small movement-based tasks through the use of fun and motivating activities that can be completed while sitting, standing or lying. A
A 




 Another
Another  The analysis was limited in many ways: for example. the highest number of studies conducted to date have been in Asia, Europe, and North America, and no studies have been reported from Africa, South America, and Australia, so this problem adversely affected the generalisability of the study results. Nevertheless, the results of this large-scale meta-analysis show that, compared to the elderly who did not receive the flu vaccine,
The analysis was limited in many ways: for example. the highest number of studies conducted to date have been in Asia, Europe, and North America, and no studies have been reported from Africa, South America, and Australia, so this problem adversely affected the generalisability of the study results. Nevertheless, the results of this large-scale meta-analysis show that, compared to the elderly who did not receive the flu vaccine,

 The Department of Computing at Imperial College London is evaluating a platform called ‘CogiGames Home’, and have asked ARNI Charity to pass this message below to stroke survivors, carers (and professionals to forward if appropriate):
The Department of Computing at Imperial College London is evaluating a platform called ‘CogiGames Home’, and have asked ARNI Charity to pass this message below to stroke survivors, carers (and professionals to forward if appropriate): 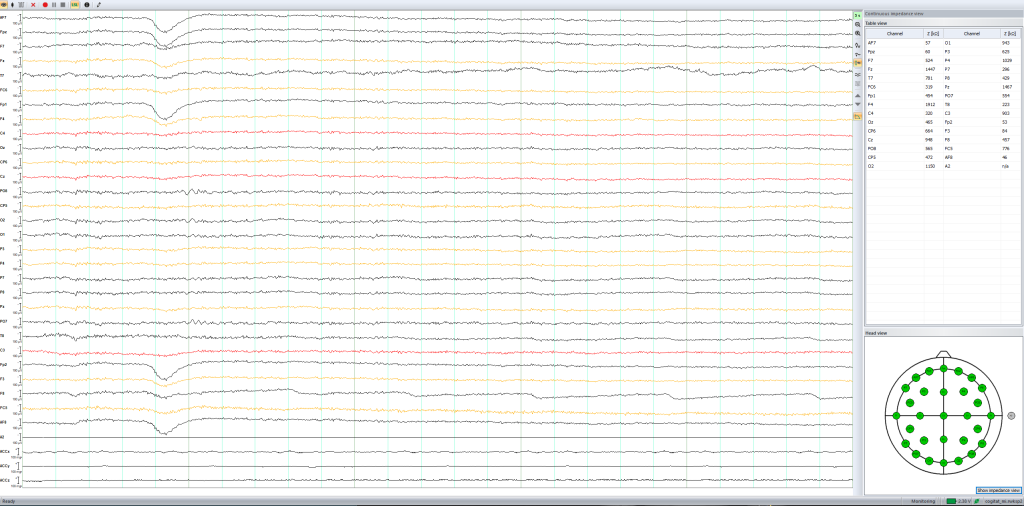




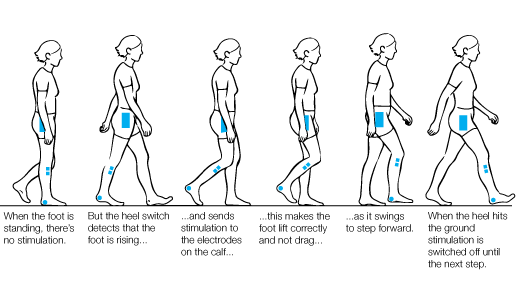
 Balance (both standing and walking) training is the only effective treatment for balance disorders, as recommended by the National Institute for Health and Care Excellence (NICE) UK
Balance (both standing and walking) training is the only effective treatment for balance disorders, as recommended by the National Institute for Health and Care Excellence (NICE) UK At University College London’s Institute of Neurology, a large-scale global research project (funded by a European Union Horizon 2021 grant), is under way (led by
At University College London’s Institute of Neurology, a large-scale global research project (funded by a European Union Horizon 2021 grant), is under way (led by 
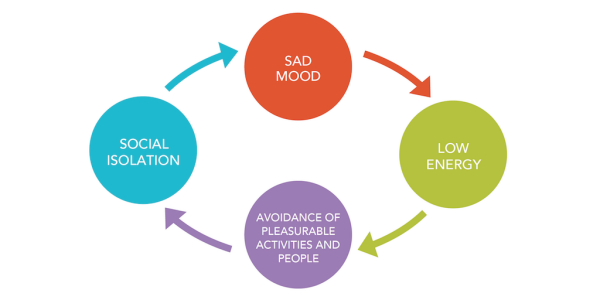

 Researchers from the Translational Neuropsychology Lab at the University of Oxford are interested in designing better treatments for depression in stroke survivors.
Researchers from the Translational Neuropsychology Lab at the University of Oxford are interested in designing better treatments for depression in stroke survivors. First, a member of the research team will contact you and see if you are eligible. This will involve them asking you some questions to make sure you are:
First, a member of the research team will contact you and see if you are eligible. This will involve them asking you some questions to make sure you are: For further help with this issue, please contact DEPRESSION ALLIANCE: A UK charity which helps people with depression, run by sufferers themselves.
For further help with this issue, please contact DEPRESSION ALLIANCE: A UK charity which helps people with depression, run by sufferers themselves. 
 The new (April 2023) stroke guidelines state (click link):
The new (April 2023) stroke guidelines state (click link):  However, access to specialist balance rehabilitation services can be poor due to the lack of enough specialists and sufficient health resources. Current programmes can be sub-optimal in that they are not truly multisensory, do not include any cognitive component (which is a key factor in determining both static and dynamic balance), and do not address real life symptoms reported by patients as challenging.
However, access to specialist balance rehabilitation services can be poor due to the lack of enough specialists and sufficient health resources. Current programmes can be sub-optimal in that they are not truly multisensory, do not include any cognitive component (which is a key factor in determining both static and dynamic balance), and do not address real life symptoms reported by patients as challenging.
 Research, led by
Research, led by 


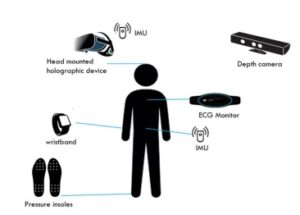 During the focus group, the team will have you watch a video which explains the HOLOBalance system. The team will then conduct semi-structured interviews related to the system usability and experience. They may also ask you additional questions as a group, to gather further feedback on the system.
During the focus group, the team will have you watch a video which explains the HOLOBalance system. The team will then conduct semi-structured interviews related to the system usability and experience. They may also ask you additional questions as a group, to gather further feedback on the system.