Arm and hand weakness is a debilitating and common consequence for a large number of stroke survivors and ARNI recognises that conventional rehab often struggles to provide the necessary intensity and engagement required to maximise the brain’s neuroplasticity.
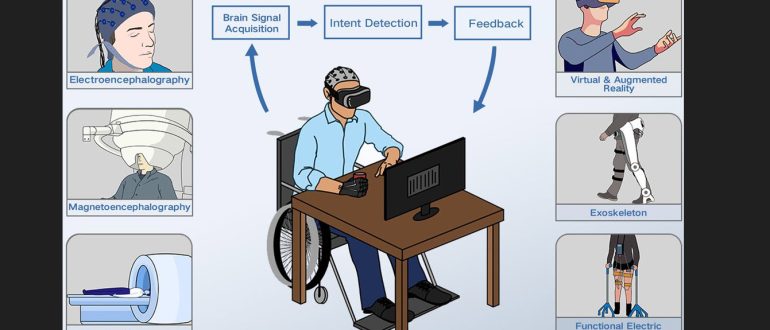
To address this problem, a team of researchers at Queen’s University Belfast’s School of Psychology, led by neuroscientist Dr. Kathy Ruddy, is conducting a new clinical trial that combines Brain-Computer Interface (BCI) technology with computer gaming to stimulate arm movement and function. This one-year project, funded by Northern Ireland Chest, Heart and Stroke (NICHS), represents a novel and potentially game-changing approach to stroke recovery.
The Queen’s University trial centres on the concept of motor imagery; research has shown that merely thinking about a movement activates the same neural pathways in the motor cortex as physically performing the action.
In the QUB trial, participants wear a simple, non-invasive BCI headset that reads their brain activity. As the stroke survivor imagines moving their affected arm, the headset detects the corresponding brain signals and these signals are then translated to control a computer game, creating a powerful biofeedback loop. This technique serves to reinforce neural pathways by repeatedly activating the motor cortex through imagined movement, allowing people with significant motor impairment to still ‘practice’ moving their arm… thereby strengthening spared neural connections/preventing from becoming dormant due to lack of use.
The trial aims to recruit 50 stroke survivors from Northern Ireland to test the efficacy of this BCI-gaming system; please contact the Queen’s University research team directly if this is of interest to you. The QUB website has a news page with contact information for the School of Psychology and research staff.