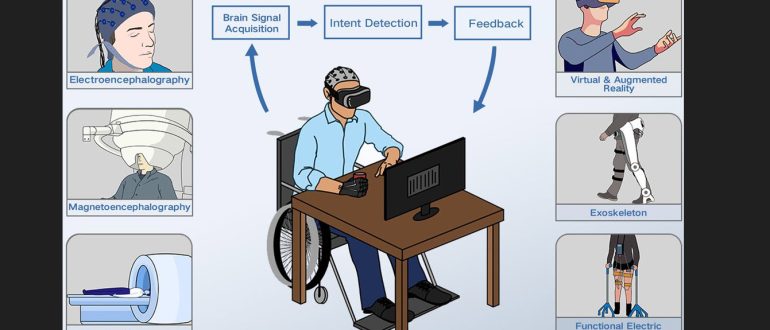
Post-stroke recovery hinges on neuroplasticity; the brain’s ability to reorganise itself to compensate for injury. Intensive, repetitive, and task-specific training is key to driving this process. Innovative VR systems, sometimes incorporating devices like the Novint Falcon haptic arm, focus on restoring specific movements, such as the pinch grip. By simulating a sense of touch, weight, and friction, it creates a more immersive and effective therapeutic environment. They provide targeted force feedback during tasks to help patients regain fine motor control.
Research using the Novint Falcon (a notable early example) and similar haptic devices has provided encouraging results. Studies have shown that haptic-enhanced VR training can significantly improve fine motor functions, hand grasping abilities, and coordination in stroke survivors, even those in the chronic stage. The device’s ability to simulate tasks like handwriting and object manipulation provides a realistic, low-cost training tool.
By integrating gamified tasks, the Novint Falcon increases patient motivation and engagement. The engaging nature of the exercises promotes higher repetition and longer training sessions, which are crucial for optimal recovery. Beyond qualitative feedback, the Novint Falcon, when integrated into a research framework, allows for the precise, objective measurement of motor performance metrics like velocity and smoothness. This data helps clinicians track progress and fine-tune therapy protocols based on an individual patient’s needs.
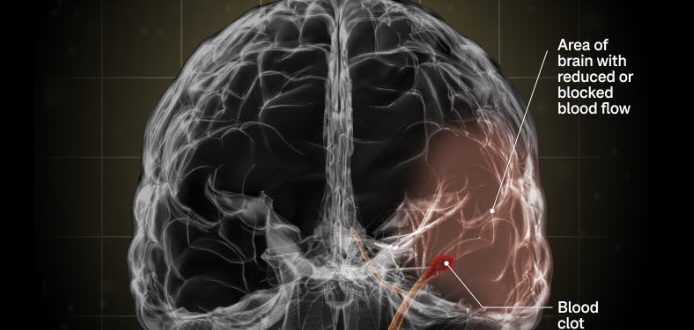
Functional Magnetic Resonance Imaging (fMRI) studies have shown that haptic-mediated therapy can induce positive cortical reorganisation in the motor cortex of stroke patients. This demonstrates that the specific feedback from the haptic device can help ‘retune’ the brain towards a more normal activation pattern.
The Novint Falcon’s relatively low cost makes it a strong candidate for at-home rehabilitation. Also, combining it with a smartphone and a custom application allows for frequent, unsupervised practice, extending the reach of therapy beyond the clinic.
While promising, more large-scale, long-term studies are needed to confirm the durability of these effects and to fully understand how haptic training translates to real-world functional tasks. Integration with other technologies and exploring applications in other sensory-motor deficits also represent exciting avenues for future research.
The Novint Falcon exemplifies how affordable, consumer-grade technology can be adapted to provide powerful therapeutic benefits. This is a step beyond passive therapy and a leap towards a more active, data-driven, and engaging future for stroke rehabilitation!